SA JOURNAL OF DIABETES & VASCULAR DISEASE
ACHIEVING BEST PRACTICE
VOLUME 7 NUMBER 2 • JUNE 2010
75
in asymptomatic diabetic patients after 2.8 years (risk ratio of
21; 95% CI: 2–204). The combination of silent ischaemia and
microalbuminuria identified a particularly high-risk group.
19
Stable angina
In patients with stable angina, it is well established that silent
ischaemia, whether present on exercise testing or Holter
monitoring, is associated with a higher risk of coronary events and
cardiac mortality.
20-22
It is, however, worth noting that the prognosis
in stable angina is relatively good once appropriate medical therapy
has been instigated. It follows that once silent ischaemia has been
detected and similar treatment commenced the prognosis should
be equivalent.
Acute coronary syndromes
The prognostic significance after MI is well known, and predischarge
exercise testing is used commonly in clinical practice. Trials have
suggested a two- to four-fold increase in cardiac events in patients
with silent ischaemia compared with those without evidence
of ischaemia.
5,6,23
The worst prognosis, however, is reserved for
patients with angina post-MI.
24
Finally, in patients with unstable
angina, one or more episodes of ST depression on 24-h continuous
ST segment monitoring was associated with a 7.43 relative risk of
cardiac death or MI at 30 days.
25
Mechanisms for the adverse prognosis
The exact reason for the poor prognosis associated with silent
ischaemia is not clear. Most likely, silent ischaemia simply confirms
the presence of significant underlying CAD. Therefore this
population is more at risk from future coronary events than those
without significant coronary disease.
In addition it is thought that repeated episodes of silent ischaemia
could do harm. They are thought to lead to progressive fibrosis,
which in turn can progress to left ventricular systolic dysfunction or
life-threatening arrhythmias. In animal models repeated transient
ischaemia is associated with sub-endocardial necrosis.
26
In humans,
myocardial biopsies fromhypokinetic territories supplied by stenosed
coronary arteries have shown areas of fibrosis and myocyte death,
in the absence of features of infarction.
27
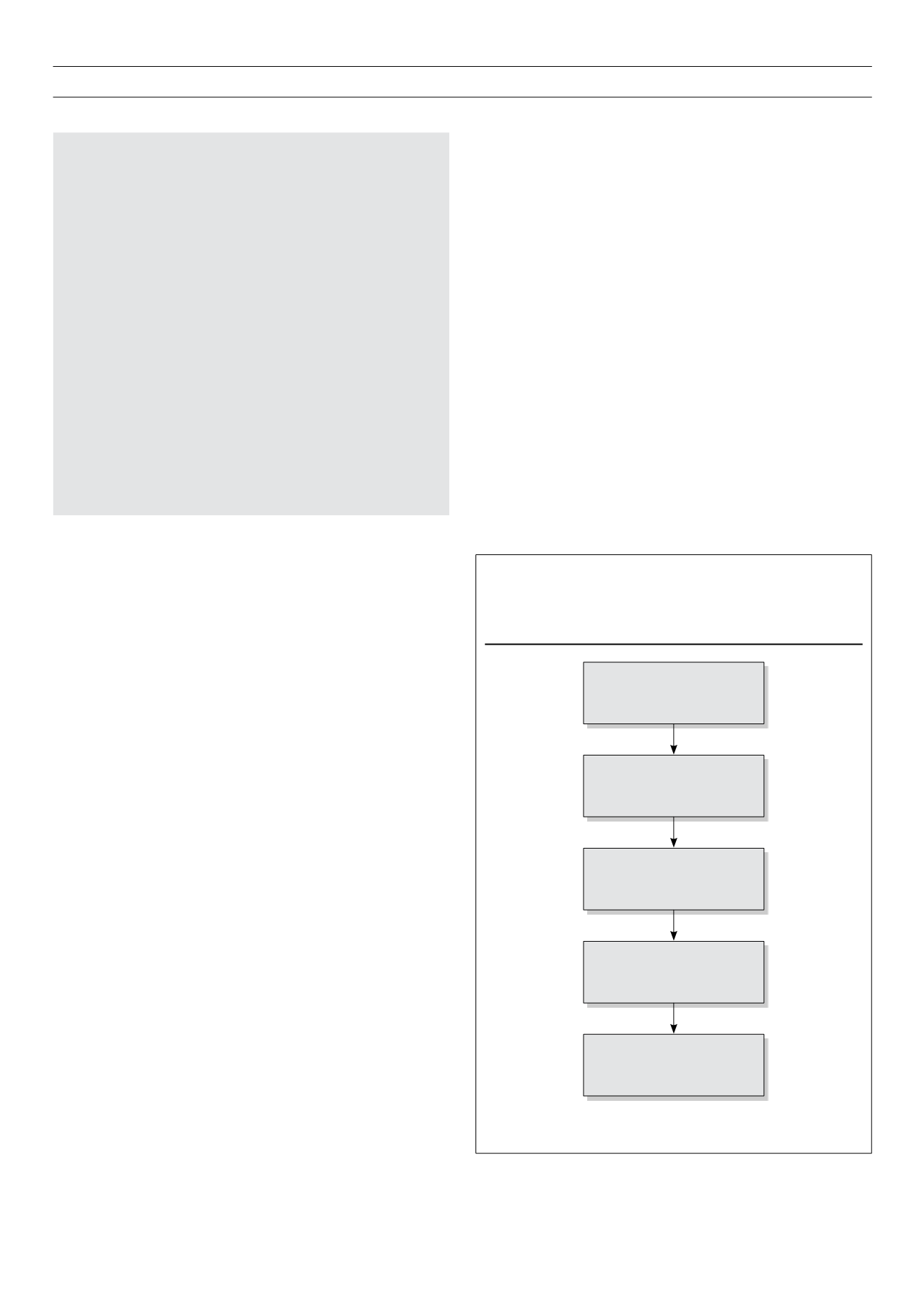
Diagnosis
The ischaemic cascade describes the sequence of events occurring
after the onset of myocardial ischaemia (Fig. 1). The perception of
pain occurs late in this sequence and is preceded first by changes
in left ventricular function and then in ECG. These two markers are
therefore a more sensitive means of detecting ischaemia than the
presence of angina.
As discussed earlier, silent ischaemia was first diagnosed using
Holter monitoring. Episodes of ischaemia are characterised by flat
or down-sloping ST depression, of at least 1 mm, which lasts for
more than 1 min and has both a gradual onset and recovery.
1,2
The most commonly used test, however, is the ETT, for which
the haemodynamic response and ST segment deviation are used
to detect underlying CAD. Indeed ambulatory monitoring does
not appear to add significantly to the findings of ETT. Transient
ischaemia on Holter monitoring appears to occur almost exclusively
in patients with a positive ETT, especially those with a positive test
at low workload.
28
However, the specificity of exercise testing is
Abbreviations and acronyms
asIsT
Atenolol Silent Ischaemia STudy
bnp
Brain Natriuretic Peptide
Cad
Coronary Artery Disease
Can
Cardiac Autonomic Neuropathy
Cards
Collaborative Atorvastatin Diabetes Study
CI
Confidence Interval
Courage Clinical Outcomes Utilizing Revascularization and Aggressive
Drug Evaluation
Ct
Computed Tomography
Danami
Danish Trial in Acute Myocardial Infarction
Diad
Detection of silent myocardial Ischaemia in Asymptomatic
Diabetics
Ecg
Electrocardiogram
Ed
Erectile Dysfunction
Ett
Exercise Tolerance Testing
Mi
Myocardial Infarction
Mrfit
Multiple Risk Factor Intervention Trial
Pvd
Peripheral Vascular Disease
Tibbs
Total Ischemic Burden Bisoprolol Study
Key:
ECG = electrocardiogram
Figure 1.
The ischaemic cascade. In the absence of angina silent ischaemia
may be diagnosed by the detection of impaired left ventricular
diastolic and systolic function on stress echo; and ECG changes
on exercise testing or Holter monitoring
Myocardial Oxygen
Supply:Demand Mismatch
Left Ventricular Diastolic
Dysfunction
Left Ventricular Systolic
Dysfunction
ECG Abnormalities
Angina