76
VOLUME 11 NUMBER 2 • JUNE 2014
REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
compensate, the pancreas releases more hormone, but eventually
fatigues, leading to insulin deficiency. Skeletal muscle
11
and liver
insulin resistance
12
have both been proposed as the primary defect
in type 2 diabetes, and the implication is that cellular insulin
resistance is the major issue.
There have been many studies investigating insulin signalling
cascades in skeletal muscle
13-15
and a variety of other cell types,
16,17
and
both receptor defects and post-receptor signalling defects have been
observed
18
yet insulin must get to the cells before it can engage the
receptors, and relies on a functioning microvasculature for access.
In the vasculature both endothelial
19-21
and vascular smooth muscle
cells
22
have shown insulin signalling defects, and functional vascular
impairments are also evident. In healthy individuals insulin signalling
in the endothelium can increase perfusion of muscle, improving the
delivery of nutrients and hormones to muscle.
23
Insulin sensitivity is
strongly related to the ability of insulin to access muscle; this access
is impaired in cases of both acute and chronic insulin resistance,
24,25
and is likely due to impaired endothelial function. Endothelial
dysfunction is evident in diabetes and even pre-diabetes,
26,27
and
men with diabetes have both impaired endothelium-dependent
and endothelium-independent vasodilation.
28
Further, endothelial
dysfunction is associated with a family history of diabetes,
29
even in
otherwise healthy individuals.
Vascular effects of exercise
Muscle is the focal point during exercise, but is also a major
metabolic organ, and the primary site for insulin-mediated glucose
metabolism. Incremental changes in exercise intensity are matched
by the amplitude increase in blood flow specifically to muscle, with
only small effects or even decreases observed in other tissues.
30
This
increase in blood flow to active tissue is termed active hyperaemia,
or functional hyperaemia. Bulk blood flow to muscle can change
significantly, particularly with exercise,
31
but the distribution of
blood through the muscle can be altered even with no changes in
total flow.
32
Light exercise in humans causes a short-term increase
in forearm blood flow within five seconds of contraction. However,
exercise also has a major effect also on microvascular blood volume,
even when the blood flow effects had returned to normal.
32
At rest,
a low proportion of capillaries are exposed to blood flow at one
time, with a rapid increase in the number of perfused capillaries
after exercise,
31
thus increasing functional capillary density. The
microvasculature in the working muscle is selectively recruited,
33
and those areas with lowest perfusion in the working muscle are
recruited first.
34
Different muscle fibres serve different roles in the
body, with highly oxidative muscle being engaged during exercise,
and glycolytic muscle fibres performing more of a postural or
structural role. Blood flow is closely coupled with the contraction of
the muscle fibres,
35
such that the magnitude of flow in each muscle
fibre type reflects activity and oxidative metabolism of the muscle.
36
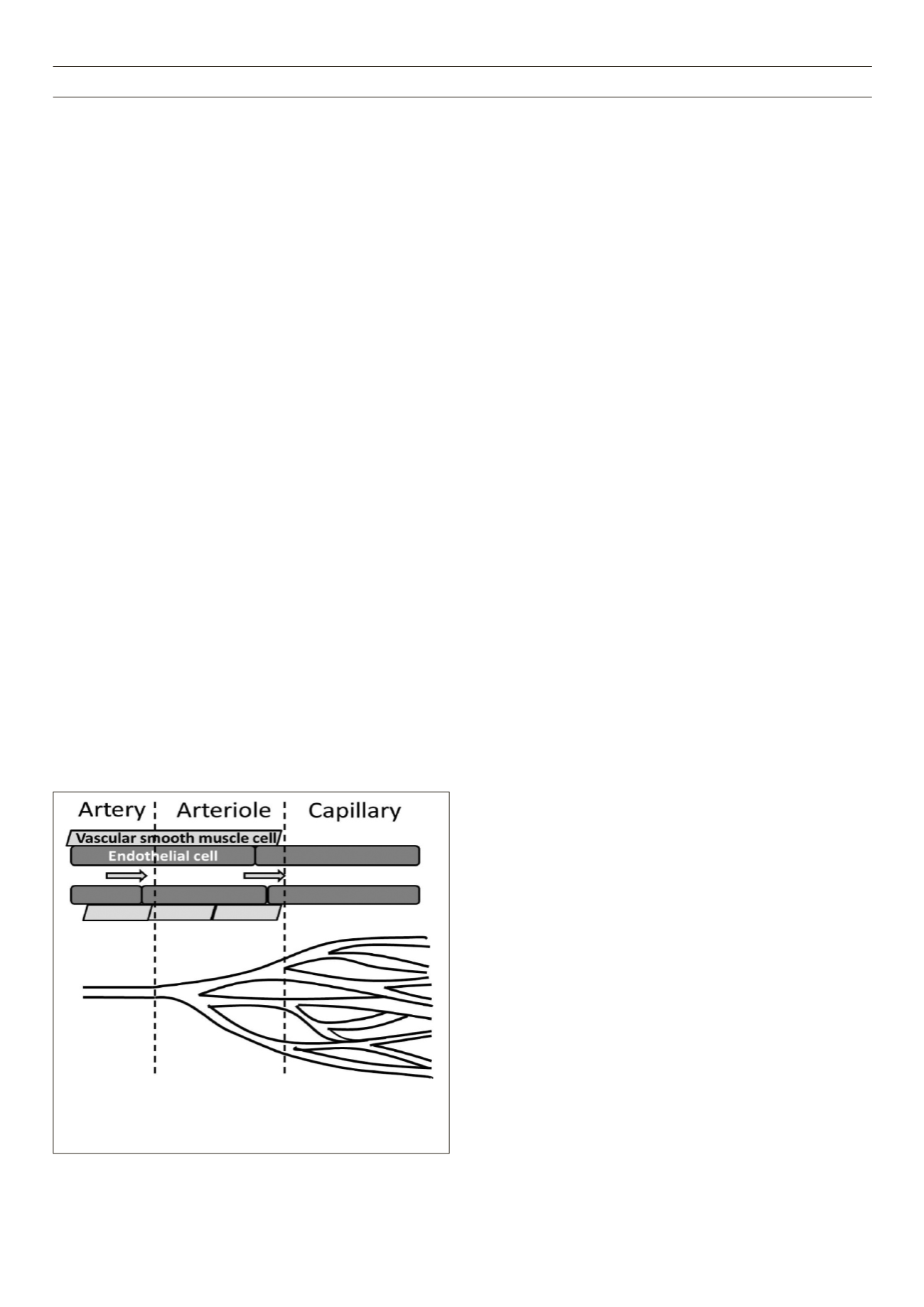
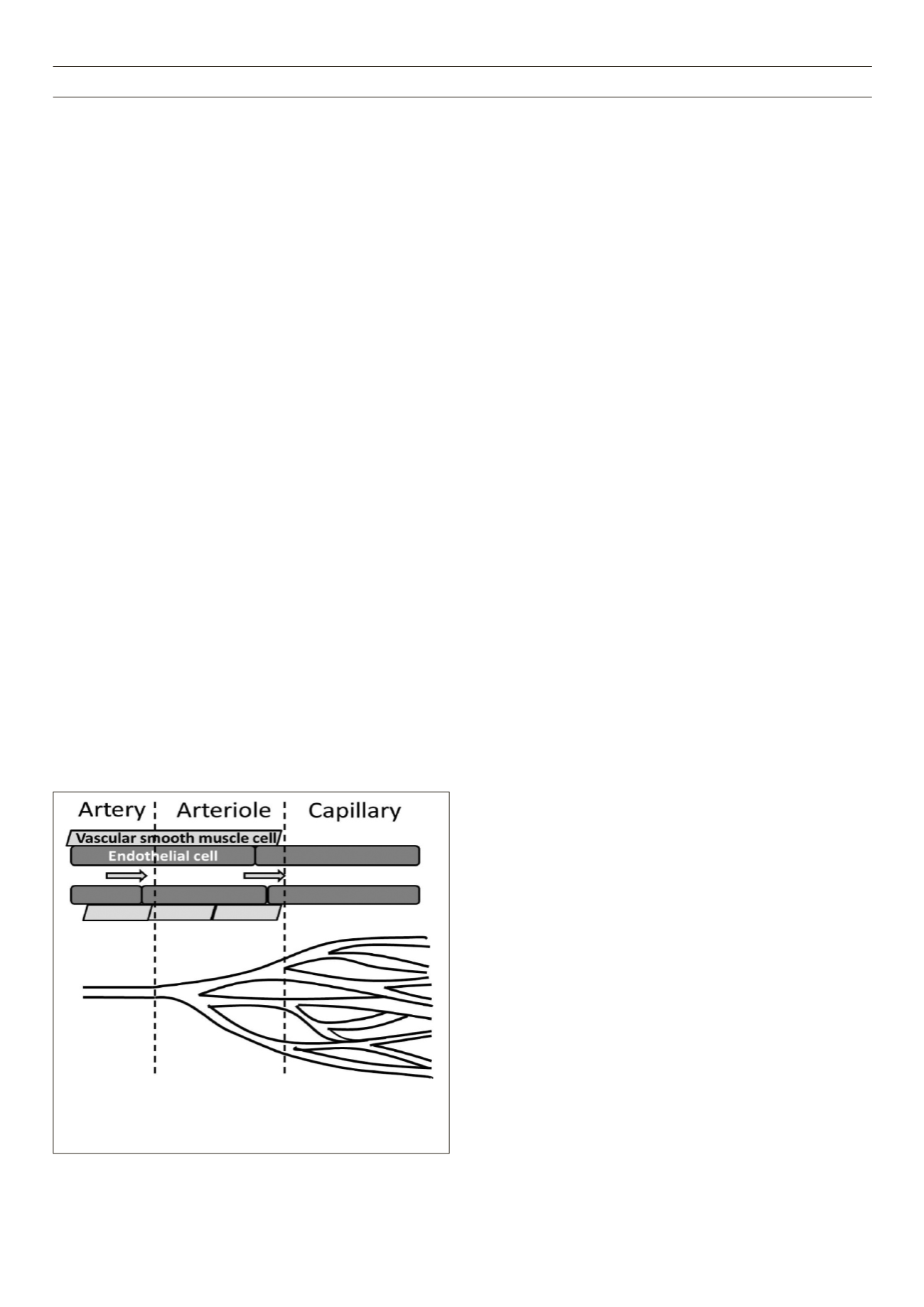
The mediators responsible for controlling muscle blood
flow during exercise can arise from the muscle, nerves and the
endothelium of blood vessels.
34,37
Vascular smooth muscle cells are
located around the arterioles and some venules, and can constrict
to change blood flow patterns, while capillaries do not typically
contribute to blood flow changes
30
(Fig. 1). Blood flow through
capillaries is controlled upstream by small arterioles at rest, and the
rapid recruitment of unperfused capillaries by exercise could suggest
that nerves are responsible for this action.
34
The sympathetic nervous
system is mainly responsible for the vasoconstrictor responses, and
as the arterioles and larger vessels are innervated,
38
the majority
of sympathetic nervous system activity is localised to that area of
the vascular tree. Physical exercise can enhance sympathetic nerve
activity39 to maintain arterial pressure, and may be involved in
maintaining exercise tolerance, as reviewed by Thomas and Segal.
38
More recent studies have suggested organ-specific differences
in sympathetic nervous system activity with weight loss.
40
While
exercise training has short-term effects to improve sympathetic
response,
39
addition of aerobic exercise to a weight-loss programme
did not augment any sympathetic changes,
41
therefore exercise
training effects on the sympathetic nervous system may be due
purely to a reduction in body weight. We suggest that short-term
effects of exercise on the sympathetic response are evident, but
the contribution of the sympathetic nervous system activity to the
beneficial effects of a long-term exercise intervention is uncertain,
and instead functional improvement of the blood vessels remains a
likely contributor to the benefits of exercise.
Insulin relies on endothelium-dependent vasodilation to enhance
perfusion, therefore endothelial dysfunction reduces insulin-
mediated increases in muscle perfusion, which can contribute to
the metabolic deficit in diabetes. As exercise-mediated changes
in perfusion are typically endothelium-independent, exercise is
still able to recruit capillaries and thus increase muscle perfusion
in obesity and type 2 diabetes, even in the face of endothelial
dysfunction. Numerous studies have now shown that while insulin’s
vascular effects may be blocked in diabetes, exercise still maintains
its ability to increase the distribution of blood flow through
muscle.
42
While physical inactivity is associated with impaired
microvascular function,
43
training programmes improve endothelial
function.
44
However, while uncomplicated type 2 diabetic patients
show normal capillary recruitment responses to exercise, in type
2 diabetic patients who also have microvascular complications,
this response is impaired,
45
likely due to a functional impairment
of blood vessels rather than morphological changes. The reduced
exercise capacity observed in type 2 diabetes subjects can be
overcome with an exercise training programme, although even
when matched for physical activity and weight, diabetic patients
have decreased physical fitness levels.
2
Figure 1.
Structural differences between artery, arteriole and capillary. No
vascular smooth muscle is located on the capillary; therefore flow through
capillaries is modified by pre-capillary arterioles. Cessation of flow through
arterioles will prevent flow through a portion of the muscle.