REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
14
VOLUME 7 NUMBER 1 • MARCH 2010
>
3.5 mg/mmol in women.
This definition takes no account of age. It is well recognised
that GFR declines with age and there is concern among some
nephrologists that a disproportionate number of elderly
people will now be inappropriately diagnosed and managed
as having CKD when their renal function is, in fact, normal
for their age.
NICE aims to minimise this risk by restricting testing for
CKD to individuals with certain known risk factors and by
specifically stating that age itself should not be seen as a risk
marker. Nonetheless, a high proportion of patients diagnosed
with CKD, or at least a finding of reduced eGFR, are elderly
and it is currently unknown whether or not these individuals
will benefit from management.
Compared to eGFR, the case for proteinuria as a marker
of systemic vascular disease, and thus a good basis for
management to reduce vascular risk, is more compelling.
The kidneys are highly vascular organs taking 25% of cardiac
output and each containing about one million glomeruli,
which are essentially knots of blood vessels. Leakage of
protein from blood vessels, such as retinal exudates in
hypertension or diabetes, has long been recognised as a
marker of systemic vascular disease and the presence of
protein in the urine is another manifestation of the same
systemic process. Proteinuria is
prima facie
evidence of harm
and thus is a strong basis for treatment, even in the elderly.
Which test should be adopted to test for proteinuria
in at-risk individuals?
ACR is the most sensitive test for proteinuria. Dipsticks are
cheap and convenient, and will detect proteinuria when
the ACR is around 45 mg/mmol. To identify individuals
with proteinuria below this level is known to be important
in people with diabetes, but there is no basis on which to
extrapolate this benefit to those without diabetes.
NICE guidance states that an ACR
<
30 mg/mmol need not
prompt a change in management in non-diabetic individuals.
So can the additional expense of ACR over dipstick be justified
in non-diabetic patients? This is a debate that is currently
unresolved. Meanwhile, testing for ACR in all patients on a
CKD register has been introduced as a performance indicator
in the 2009 Quality and Outcomes Framework (QOF).
Practicalities of testing for CKD
NICE guidance states that testing for CKD should be offered
to patients with the following risk factors:
hypertension
•
cardiovascular disease
•
renal stone disease or prostatic problems
•
known multisystem disease with potential for renal
•
involvement
family history of CKD
•
incidental finding of haematuria or proteinuria.
•
Even though it is stated in NICE guidance that advanced
age should not be considered a risk factor, there is a high
proportion of the elderly population in these at-risk groups.
Practitioners are therefore encouraged to take account
of age and co-morbidity (and thus likely prognosis) before
incorporating the elderly into management programmes. No
clear guidance can be given on this matter: it is a distillation
of common sense, experience and good clinical judgement.
However, a competent medical evaluation is required rather
than a protocol-driven pathway.
eGFR estimations can fluctuate, particularly when eGFR
is just below the normal range (eGFR 45–60 ml/min). It is
therefore important to minimise these fluctuations by asking
patients to abstain from meat for 12 hours before collecting
a urine sample and to maintain hydration with clear fluids.
Patients attending for fasting blood tests often think they
should take ‘nil by mouth’ and so are tested when relatively
dehydrated.
The initial screen for proteinuria does not require an early
morning sample. However, if initial ACR is 30–70 mg/mmol,
a repeat test using an early morning sample is advised as
minor proteinuria may be increased into the abnormal range
by exercise and orthostasis. If the initial sample shows ACR >
70 mg/mmol, this is likely to represent significant proteinuria
requiring intervention. Proteinuria is also increased in the
presence of hypertension and one might expect the ACR to
fall once blood pressure has been brought under control.
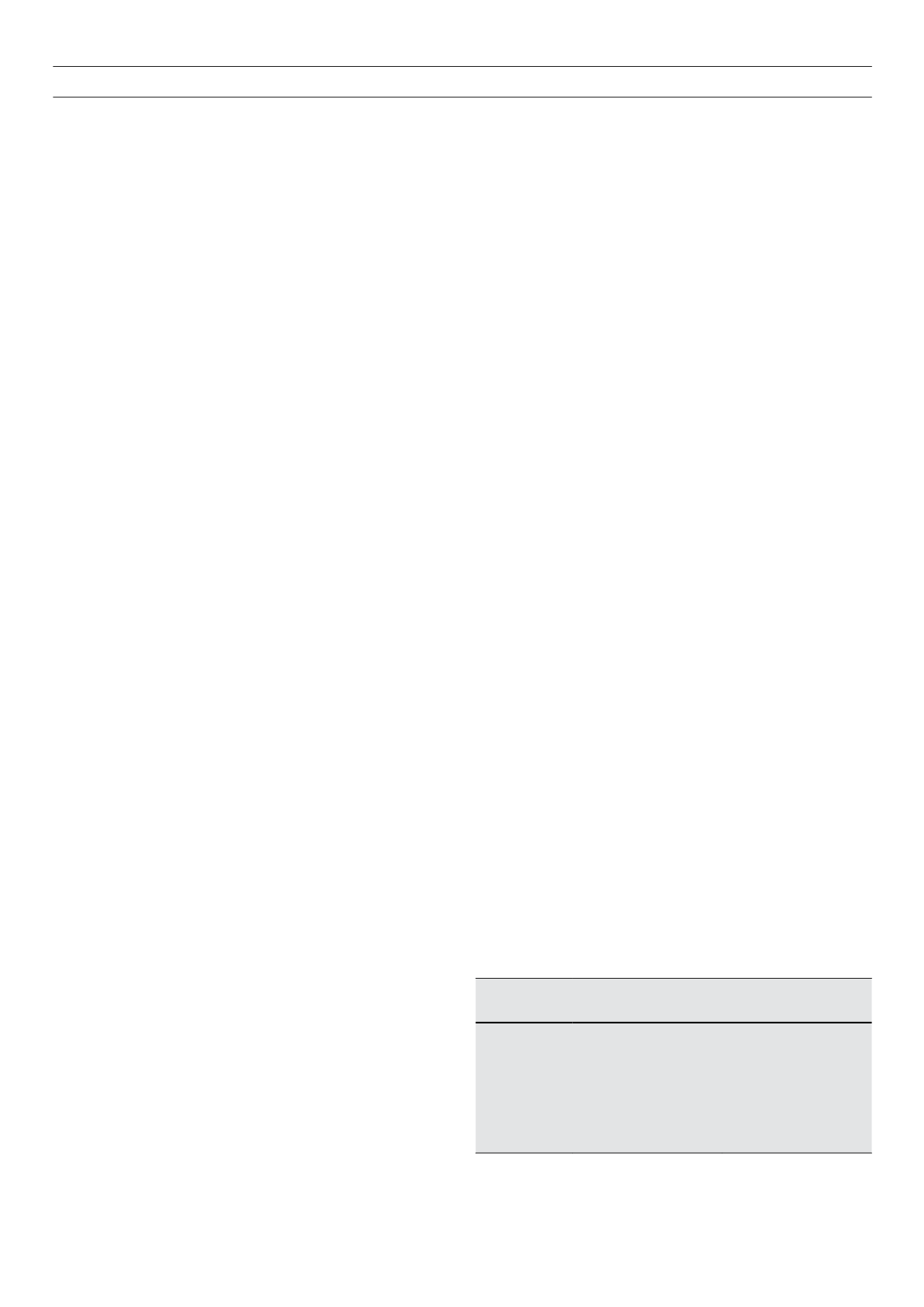
Monitoring CKD
The testing frequency recommended by NICE is outlined in
Table 2. Most individuals with stage 4–5 CKD will be under
the care of the specialist renal service. However, elderly
patients with eGFR
<
29 ml/min are frequently identified
who have very stable eGFRs and show no trajectory towards
end-stage renal failure. These might opt to be monitored as
outlined in Table 2 in a primary care setting, with referral
should their function be seen to decline.
ThemainpurposeofmonitoringCKDistoidentifyindividuals
with progressive CKD, who are at risk of developing end-
stage kidney disease within their expected natural lifetime. It
is important to realise that even with optimal management,
CKD is a progressive disease. Management may slow decline
but failure to halt progression does not necessarily mean that
treatment has been sub-optimal or ineffective.
NICE defines progressive CKD as a decline in eGFR of
>
5ml/
min/1.73 m
2
in one year (or 10 ml/min/1.73 m
2
in five years).
Table 2.
Stages of CKD and frequency of eGFR testing
CKD stage
eGFR (ml/min)
Frequency of monitoring
1 and 2
>
60
Annually
3A and 3B
30–59
6-monthly
4
15–29
3-monthly
5
<
15
4–6-weekly
CKD
=
chronic kidney disease; eGFR
=
estimated glomerular filtration rate