SA JOURNAL OF DIABETES & VASCULAR DISEASE
ACHIEVING BEST PRACTICE
VOLUME 7 NUMBER 1 • MARCH 2010
25
by the Trust’s Drug and Therapeutics Committee. Unless there
was a clear contraindication, ACE inhibitors or ARBs were
used as first-line drugs if the patient was not prescribed these.
The use of irbesartan was favoured in our clinic because of its
evidence base
3,4
and was included in the clinic protocol prior
to publication of further evidence supporting similar effects
with ACE inhibitors.
5
Ramipril was the preferred choice of
ACE inhibitor for primary care and perindopril for hospital.
Doses were maximised if possible, and other antihypertensive
drugs added as necessary, taking into account tolerance, any
co-morbidities and contra-indications. Titration and drug
additions were made four times weekly, and compliance and
side-effect issues were always discussed. The nurse worked
alone, but problems were discussed as necessary with the
supervising consultant physicians (GVG and JPW).
Biochemical measurements
At entry to the clinic, glycated haemoglobin, non-fasting
serum total and HDL cholesterol, serum creatinine, eGFR
and urinary albumin:creatinine ratio were measured by
standard laboratory techniques. Biochemical measurements
were undertaken at Aintree University Hospital biochemistry
department. These were repeated at the 12-month review.
Demographic data including body mass index were also
recorded. If ACE inhibitor or ARB drugs were being
commenced, or doses increased, biochemical renal function
and electrolytes were measured one week later.
Statistics
Data were recorded and transferred to an
Excel
spreadsheet.
Statistical analyses were undertaken using a
StatsDirect
Biomedical Software
package (StatsDirect, Sale, Cheshire,
UK). Student’s paired or unpaired
t
-test compared quantitative
data. Proportionate data were analysed using a Chi-squared
or Fisher’s exact test. Comparisons of systolic and diastolic BP
over time were assessed by analysis of variance (ANOVA).
Results
Patient numbers and characteristics
There were 104 patients referred to the clinic. Of these, 71
completed all appointments and the 12-month review visit.
The remaining 33 included seven who died during follow-up,
and 26 (25%) who failed to attend (in five this was because
of repeated hospital admissions). Of the 71 patients who
completed the study, 52 (72%) had microalbuminuria and
19 (28%) had nephropathy. Comparing the characteristics
of these two groups, there were no significant differences.
Mean (
±
SD) age was 62
±
1 years in the microalbuminuria
group and 64
±
11 years in the nephropathy group. Diabetes
duration was 8
±
6 versus 10
±
7 years, male:female ratio
75:25% versus 68:32%, body mass index 34
±
5 versus 34
±
11, insulin treatment 46% versus 37%. Large vessel disease
was common, i.e. ischaemic heart disease 29% versus 32%,
cerebrovascular disease 6% versus 16%, and peripheral
vascular disease 15% versus 32%.
Clinic progress
There was a reduction in BP noted between the referral
routine diabetic clinic visit, and the first nurse-led clinic
Table 2.
Comparison of microalbuminuria group in 52 patients with data both
at entry and review (
n
=
52)
Characteristic
Entry Review
p
-value
Blood pressure
≤
130/80 mmHg
13 (25%)
30 (58%)
p
=
0.001*
Urinary albumin:creatinine ratio (mmol/l)
†
8.4
±
5.3
(n
=
49)
4.6
±
4.2
(
n
=
36)
‡
p
=
0.0003
Creatinine (mmol/l)
94
±
20
109
±
28
(
n
=
44)
p
<
0.0001
ARB/ACE inhibitor
34 (65%)
48 (92%)
p
=
0.001*
Microalbuminuria
†
52 (100%) 39 (75%)
p
=
0.0001*
eGFR (ml/min)
82
±
22 72
±
22
p
<
0.0001
Three or more antihypertensive drugs
14 (27%)
27 (52%)
p
=
0.02
Glycated haemoglobin (%)
8.6
±
1.4
7.9
±
1.8
(
n
=
39)
p
=
0.01
Total cholesterol (mmol/l)
4.8
±
1.0 4.2
±
0.9
p
<
0.0001
HDL cholesterol (mmol/l)
1.2
±
0.2 1.1
±
0.2
p
=
0.02
Statin
40 (77%)
51 (98%)
p
=
0.002*
Antiplatelet
36 (69%)
49 (94%)
p
=
0.002*
P
-values by Chi-squared test and Fisher’s exact test* for categorical variables and
paired
t
-test for continuous variables unless stated
Data given as
n
(%) for categorical variables and mean
±
SD for continuous
variables
† Albumin:creatinine ratio levels
>
2.5 mg/mmol in men and
>
3.5 mg/mmol in
women
‡ Two (4%) patients progressed to nephropathy
ACE inhibitor
=
angiotensin converting enzyme inhibitor; ARB
=
angiotensin
receptor blocker; eGFR
=
estimated glomerular filtration rate;
HDL
=
high-density lipoprotein
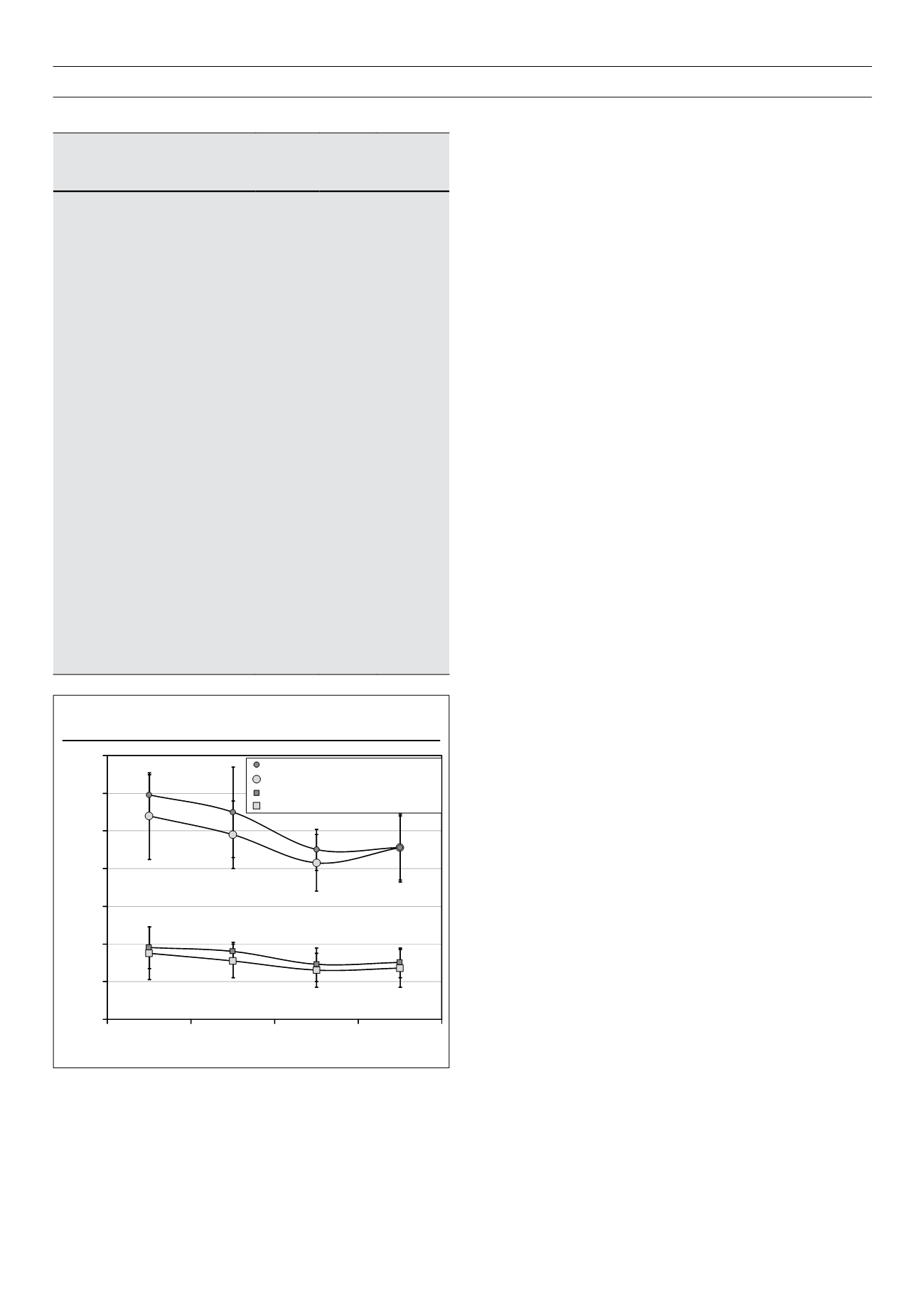
Figure 2.
Blood pressure control from entry visit to review visit
40
60
80
100
120
140
160
180
Entry
First visit
Exit
Review
Blood pressure (mmHg)
SBP nephropathy:
p
< 0.0001
SBP microalbuminuria:
p
< 0.0001
DBP nephropathy:
p
< 0.0004
DBP microalbuminuria:
p
< 0.0001
Values are means
±
S
D