SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 7 NUMBER 3 • SEPTEMBER 2010
97
drugs (bevacizumab, ranibizumab or pegaptanib) for their anti-
permeability and anti-angiogenic effects on decreasing macular
oedema and neovascularisation. These drugs have a temporary
effect though and repeated injections (with associated risks – Table
5) are necessary. As an adjunct to laser or vitrectomy techniques,
these drugs are showing excellent results.
15
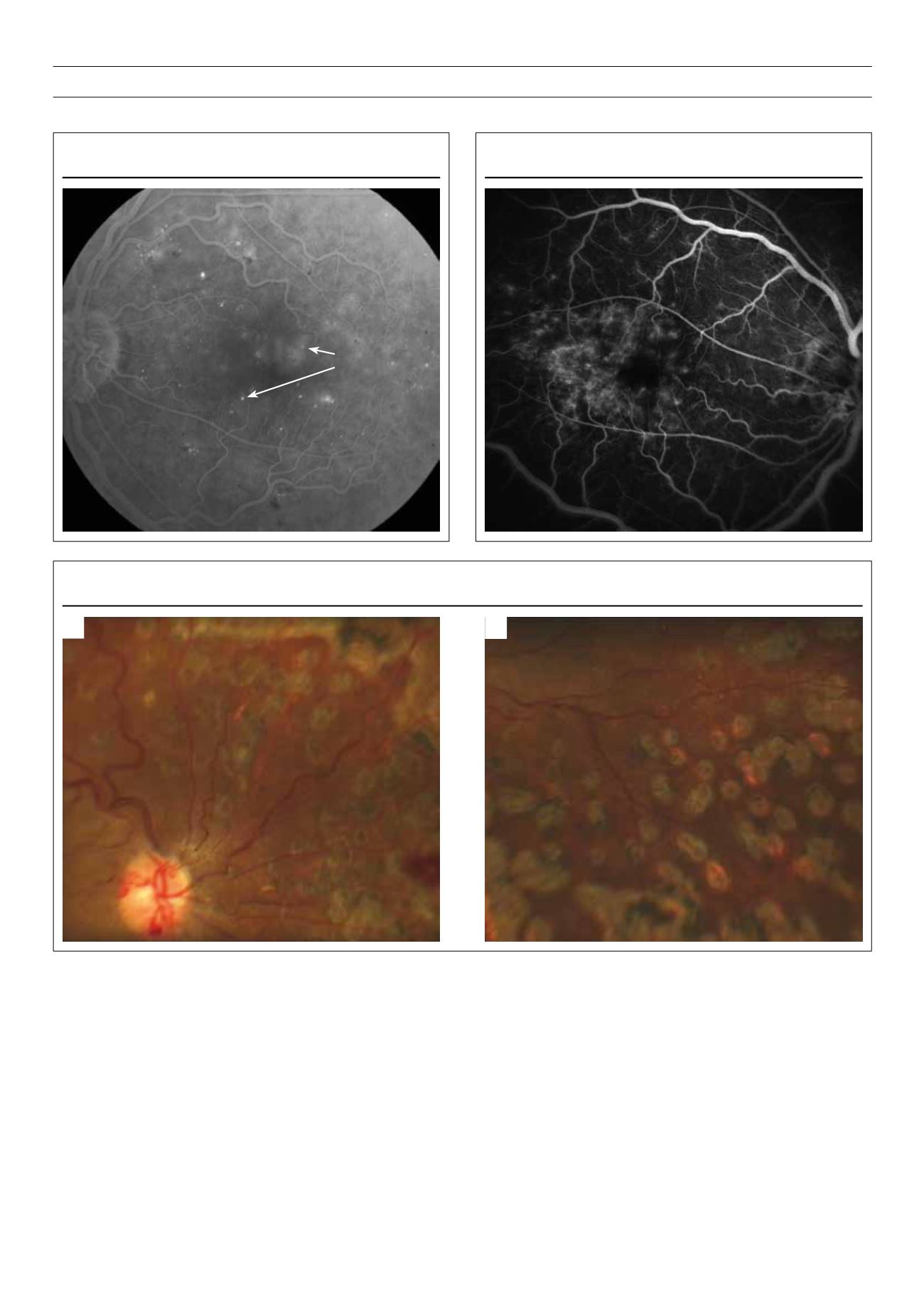
Laser techniques can be classified as pan-retinal, focal, or grid.
Pan-retinal laser, also referred to as scatter laser, is used for the
treatment of proliferative diabetic retinopathy and indirectly treats
neovascularisation of the optic nerve, retinal surfaces, or in the
anterior chamber angle by placing laser burns throughout the
peripheral fundus. This ablation of the ischaemic peripheral retina
leads to a decrease in the production of vascular endothelial growth
factor (VEGF), which in turn leads to regression of the new vessels
(Figure 10a, b). It may be done in more than one session.
Focal and grid laser are used for the treatment of diabetic
macular oedema. Focal laser applies light, small-sized burns to
leaking micro-aneurysms in the macula, and grid laser applies a grid
or pattern of burns (mimicking pan-retinal laser but using smaller
burns) to the areas of macular oedema arising from diffuse capillary
leakage.
The goal of laser surgery is to reduce the risk of visual loss rather
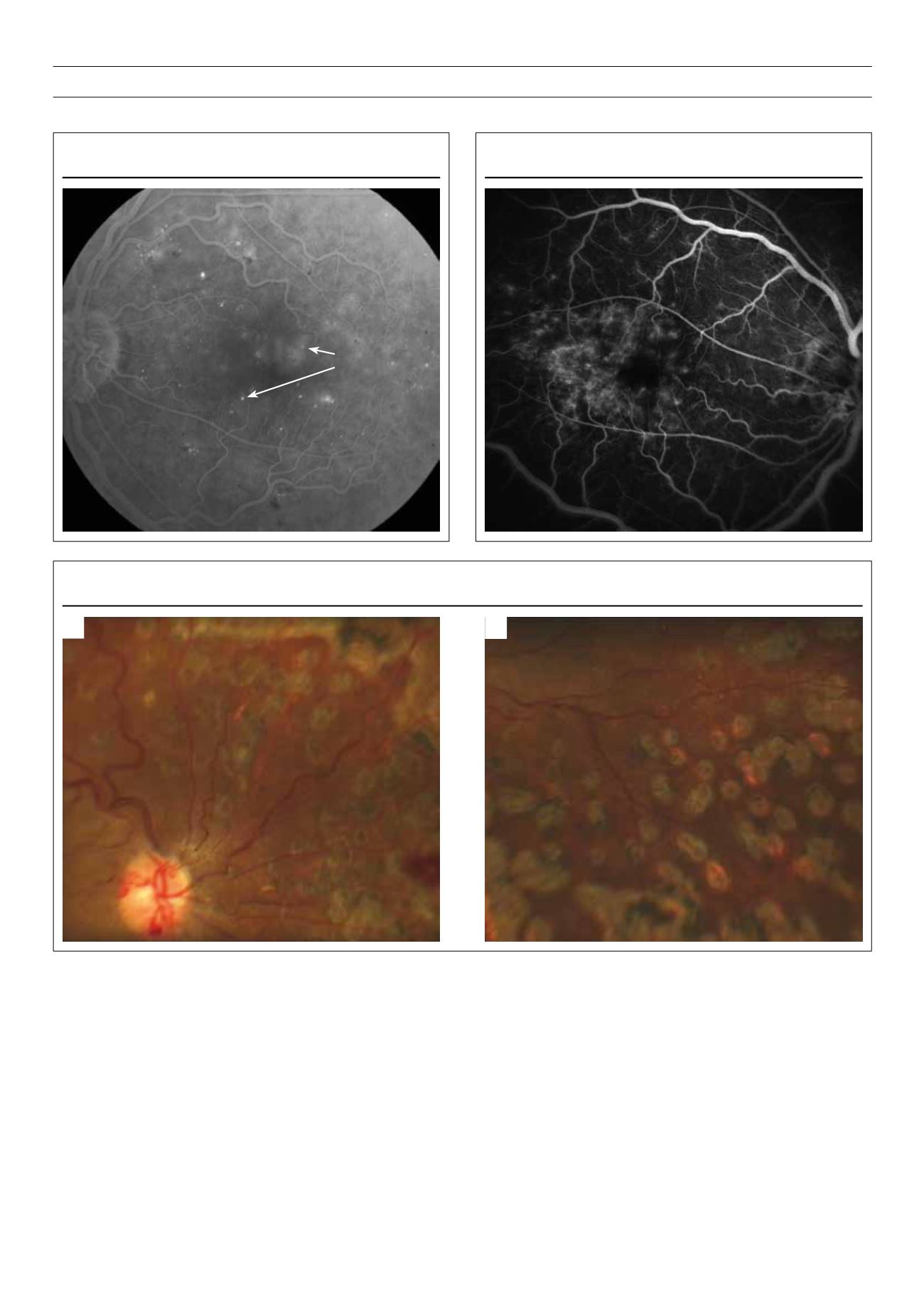
Figure 9.
FFA showing diffuse macular oedema amenable to grid laser.
Figure 8.
FFA showing focal leakage amenable to focal laser.
Macular oedema
Micro-aneurysms
Figure 10.
Scatter laser scars
A
B
Right
Left