SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 7 NUMBER 3 • SEPTEMBER 2010
95
Early detection of retinopathy depends on educating patients
with diabetes as well as their families and healthcare providers
about the importance of regular eye examination even though
the patient may be completely asymptomatic. Treatment can yield
substantial cost savings compared with the costs for those disabled
by vision loss. Analyses from the DRS, ETDRS and DRVS trials
showed that the treatment for diabetic retinopathy may be 90%
effective in preventing severe vision loss using current treatment
strategies.
11
Although effective treatment is available, their primary-care
physicians for ophthalmic care refer far fewer patients with diabetes
than would be expected. Even in a first-world environment such as
the USA, it was found that less than 50% of diabetics underwent
an annual eye examination.
12
In South Africa, where the burden of
disease is very high and the numbers of ophthalmologists are low,
it is likely that only 10% of patients receive eye examinations at the
appropriate intervals.
There are numerous screening programmes in existence
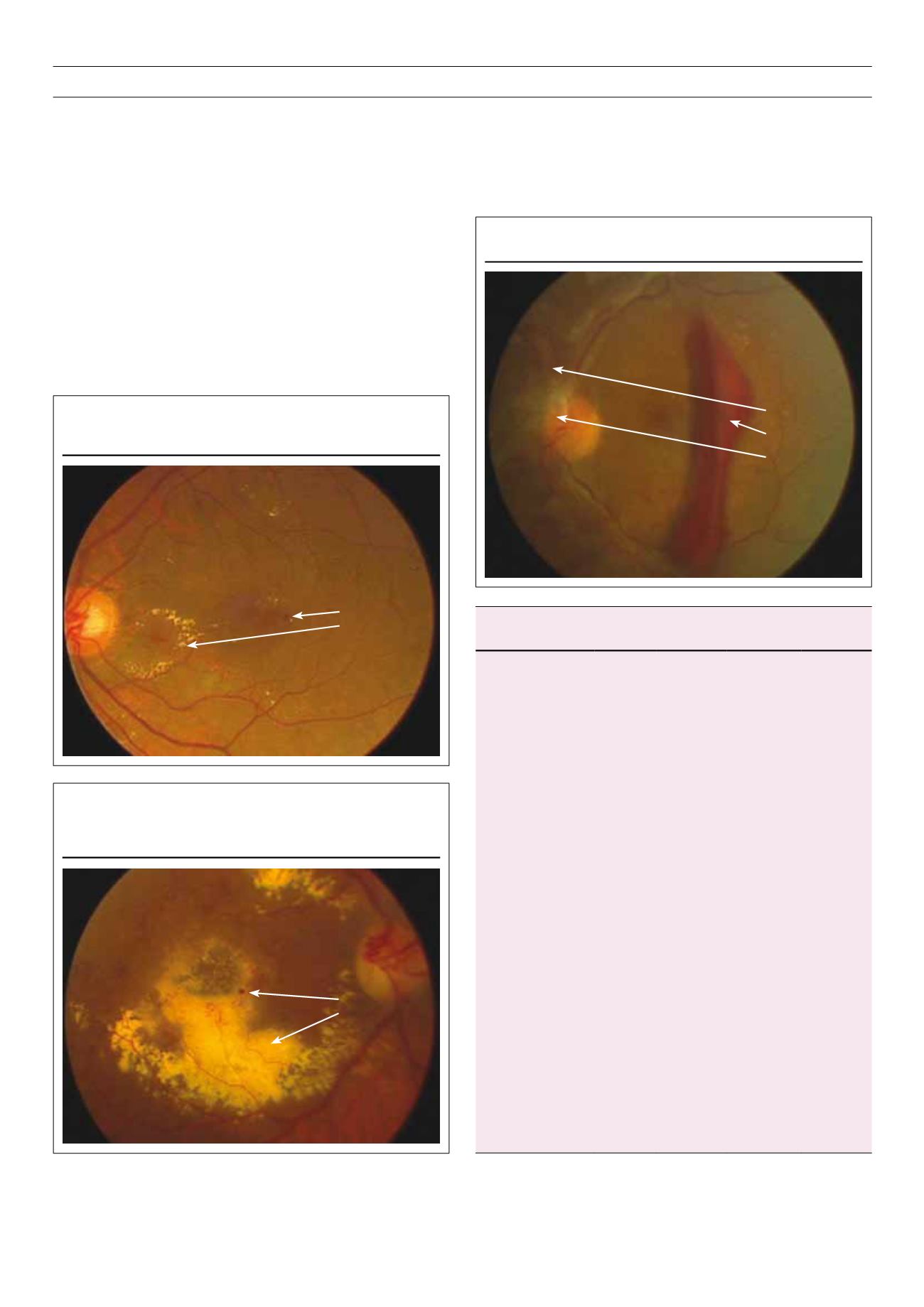
Figure 3.
Proliferative diabetic retinopathy.
New vessels
Pre-retinal
haemorrhage
Gliosis (fibrosis)
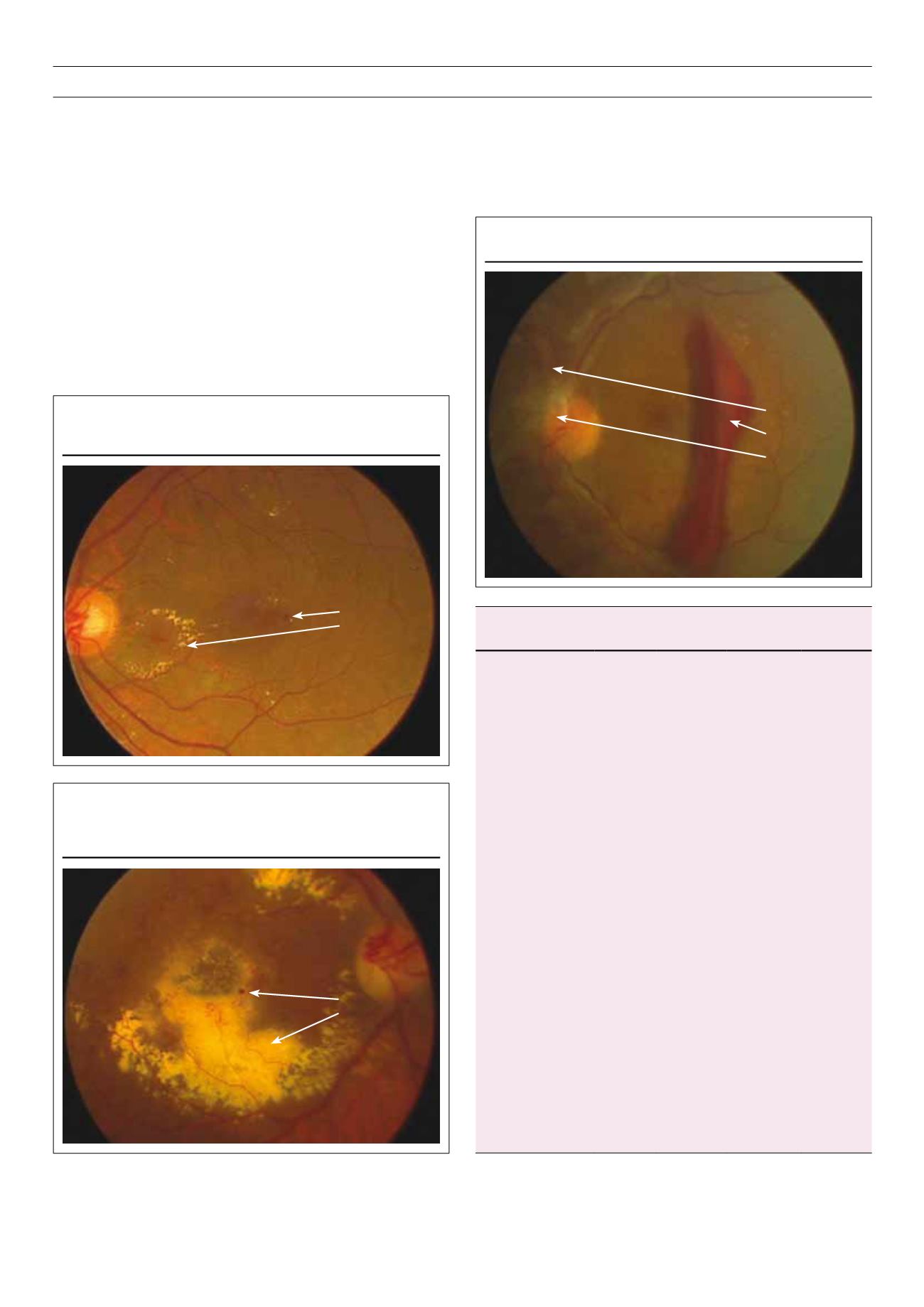
Figure 1.
Moderate non-proliferative diabetic retinopathy with
maculopathy.
Micro-aneurysms
Hard exudates
Figure 2.
Moderate non-proliferative diabetic retinopathy with massive
macular exudation in a patient with hypertension and
hyperlipidaemia.
Micro-aneurysms
Hard exudates
Table 4.
Management recommendations for patients with diabetes
Severity of
retinopathy
Presence
of CSME
Follow-up
(months)
Pan-retinal
laser
Focal and/
or grid
laser*
1. Normal or minimal
NPDR
No
12
No
No
2. Mild to moderate
NPDR
No
Yes
6–12
2–4
No
No
No
Usually**
3. Severe NPDR
No
Yes
2–4
2–4
Sometimes
+
Sometimes
+
No
Usually
‡
4. Non-high-risk PDR No
Yes
2–4
2–4
Sometimes
+
Sometimes
+
No
Usually**
5. High-risk PDR
No
Yes
2–4
2–4
Usually
Usually
No
Usually
‡
6. Inactive PDR
No
Yes
6–12
2–4
No
No
No
Usually
CSME
=
clinically significant macular oedema; NPDR = non-proliferative
diabetic retinopathy; PDR
=
proliferative diabetic retinopathy.
*Adjunctive treatment, which may be used include intra-vitreal steroids or
anti-vascular endothelial growth factor (VEGF) agents (off-label use).
**Deferring treatment is an option when the centre of the macula is not
involved, close-up follow-up is possible if the patient understands the risk.
Treatment is more likely to stabilise vision, but treatment close to the fovea
may result in damage to central vision and, with time, scars may expand and
cause further deterioration of vision.
+
Benefit of early pan-retinal laser at severe NPDR or non-high-risk PDR
stages is greater in patients with type 2 diabetes. Other factors such as poor
compliance, impending cataract surgery or pregnancy and status of the
fellow eye will help in determining the timing of the laser.
‡
Preferable to perform focal laser first, prior to pan-retinal laser to minimise
pan-retinal laser-induced exacerbation of the macular oedema.