VOLUME 7 NUMBER 3 • SEPTEMBER 2010
125
SA JOURNAL OF DIABETES & VASCULAR DISEASE
ADA WATCH
a low sensitivity of detecting the onset of
both diabetes and pre-diabetes, as defined
by previous definitions of diabetes, using
fasting glucose values (
≥
11.1 mmol/l),
impaired glucose tolerance (IGT) (2-h glu-
cose: 7.8–11.0 mmol/l) and impaired fast-
ing glucose (IFG) (fasting glucose: 5.6–6.9
mmol/l).
The sensitivity and specificity of HbA
1c
≥
6.5% for detecting incident diabetes was
22 and 99.5%, respectively. The low sen-
sitivity of these HbA
1c
cut-off points could
jeopardise the timely implementation of
protective lifestyle and pharmacological
interventions.
Source: Presidents Poster, 0424-PP. Haffer SM,
Wagenknecht LE, Hanley AJ,
et al
. HbA
1c
and fasting
and 2-h glucose concentrations for detecting worsening
of glucose tolerance status in individuals with normal
glucose tolerance at baseline: the Insulin Resistance
Atherosclerosis Study.
New metabolic syndrome definition
and value of waist circumference
evaluated in type 2 diabetes
The recent consensus definition of the
metabolic syndrome allows for both the
IDF and NCEP ATP III cut-off points for the
diagnosis of a large waist in Caucasians. Its
value in predicting type 2 diabetes has not
yet been assessed.
This prospective study assessed and fol-
lowed up for eight years, more than 500
non-diabetic Caucasians undergoing coro-
nary angiography for evaluation of stable
CAD. At baseline, 50% of the patients met
the novel consensus metabolic syndrome
definition but the predictability of this defi-
nition was enhanced when the NCEP ATP III
waist circumference cut-off values of more
than 102 cm for men and more than 88 cm
in women were used.
The eight-year incidence of type 2 diabe-
tes was 32% in patients defined according
to these criteria, compared to 15% using
the smaller waist circumference measure.
Source: Abstract 0381-OR. Saely CH, Vonbank A,
Rein P,
et al
. Prediction of type 2 diabetes with the
novel metabolic syndrome consensus definition: The
importance of waist circumference.
Diabetes therapy
Metformin protects against anti-
depressant diabetes risk?
Continuous use of antidepressant medi-
cation increased the risk of developing
diabetes in the 10 years of the extended
Diabetes Prevention Programme Outcomes
Study (DPPOS) in those patients not receiv-
ing metformin. There was no association
between antidepressant medication usage
and diabetes risk in patients receiving met-
formin.
This ADA-sponsored research confirms
the strong positive and statistically signifi-
cant association between continuous anti-
depressant medication use and increased
diabetes risk found in the three-year fol-
low-up period of the DPP in those patients
on the placebo and intensive lifestyle arm.
The researchers noted that this association
was still significant when controlled for
depression symptom level.
While acknowledging that this find-
ing does not allow the interpretation of a
protective effect of metformin, it does alert
clinicians to the higher diabetes risk facing
patients who are being treated also for
long-term depression.
Source: Presidents Poster. Abstract No 0479-PP. Rubin
RR, Marrero DG, Yong MA,
et al
. Antidepressant
medication use and risk of developing diabetes during
the Diabetes Prevention Program and the Diabetes
Prevention Programme Outcomes study.
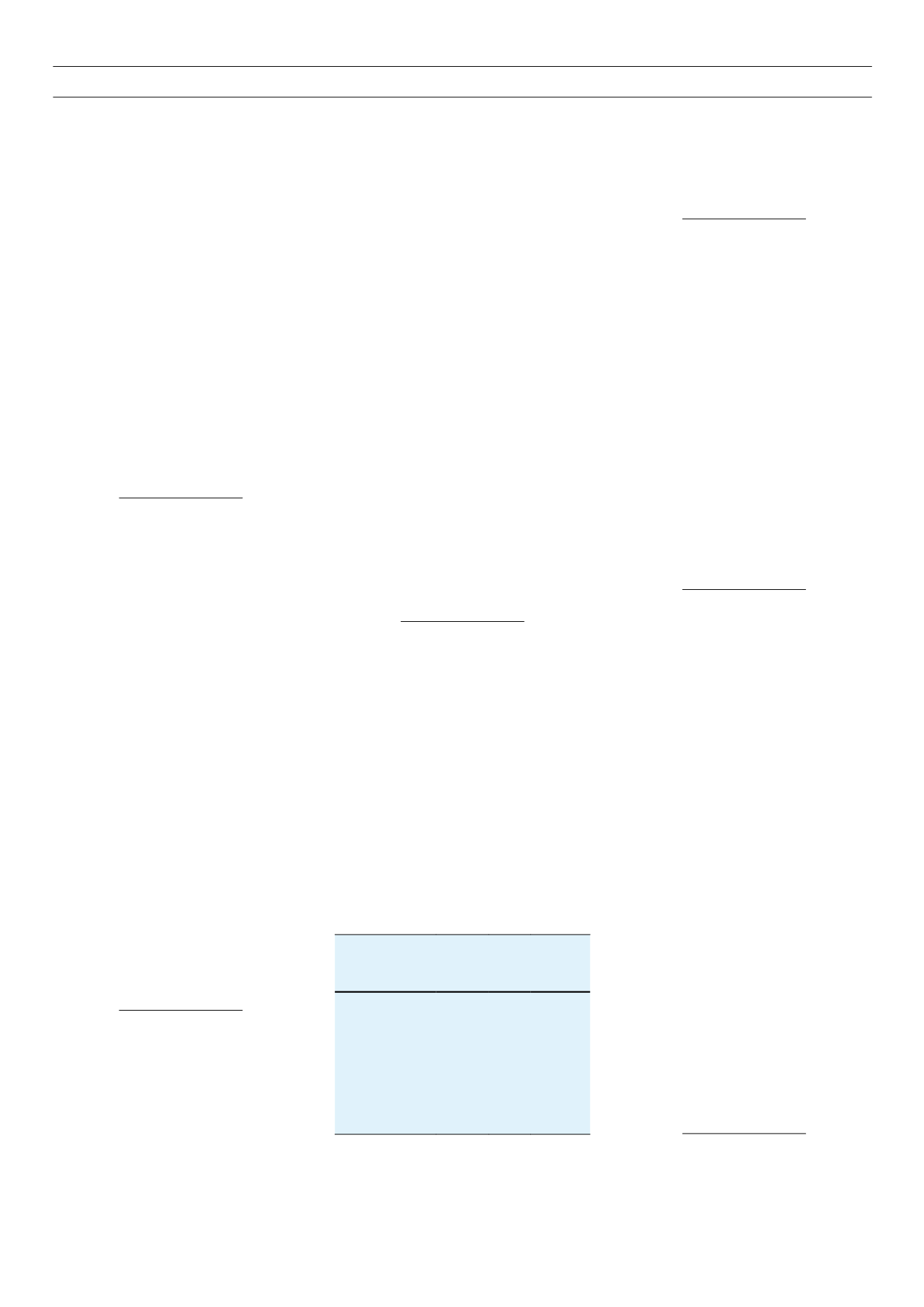
Once-daily liraglutide lowers
systolic blood pressure (SBP) in
treated and untreated hypertensive
patients
A meta-analysis of six randomised, control-
led trials (
n
=
3 967) has shown that the
reduction in SBP with liraglutide was inde-
pendent of concomitant antihypertensive
treatment (AH), and that this reduction
was additive to concomitant antihyper-
tensive therapy. The evaluation was done
using an ANCOVA model, which included
randomised treatment effect, use of AH
therapy at 26 weeks and interaction with
liraglutide/placebo at 26 weeks.
Source: Abstract 0296-OR. Fonseca V, Plutzky J,
Montanya E,
et al
. Liraglutide, a once-daily human
GLP-1 analog, lowers systolic blood pressure (SBP)
independently or concomitant antihypertensive treat-
ment.
Dietary omega-3 polyunsaturated
fatty acid (fish oil capsules) reduced
atherosclerosis progression in type
2 diabetes
This one-year study of 300 patients with
type 2 diabetes showed that carotid
intima–media thickness did not progress
in patients receiving fish oil capsules, com-
pared to patients following the diet recom-
mended by ESC/EASD.
The dosage of omega-3 was 1 g EPA,
1 g DHA and 0.1 g alpha-tocopherol ace-
tate. Interestingly, total cholesterol, HDL
cholesterol and triglyceride levels improved
in those patients on the fish oil capsules.
Source: Abstract 0193-OR. Dragomir AD, Radulian
G, Rosu E,
et al.
One-year administration of dietary
omega-3 polyunsaturated fatty acid decreases oxidative
stress and atheroscerlosis progression in type 2 diabetes.
Costs of continuing sulphonyl-
ureas with insulin therapy in type 2
diabetes: more hypoglycaemia and
weight gain but less insulin needed
There is no consensus on whether insulin
secretagogues should be maintained when
analogue insulin therapy is added to the
type 2 diabetes regimen, while metformin
is continued.
This multinational study of almost 1 000
insulin-naïve patients tracked diabetes
control when basal insulin (glargine once
daily or detemir twice daily) was added and
sulphonylureas and glinides were retained/
stopped.
Glucose control was not statistically
significantly different but patients who
continued with sulphonylureas had more
hypoglycaemia (40 vs 24.5%) and gained
significantly more weight (1.5 vs 0.4 kg).
End-of study daily insulin doses were how-
ever significantly lower in patients continu-
ing secretagogues than in those stopping
these agents (0.6 vs 0.8 units/kg/day).
Source: Abstract 0037-OR. Swinnen SG, Dain MP,
Mauricio D,
et al
. Continuation versus discontinuation
of insulin sceretagogues when initiating insulin in type
2 diabetes
.
Table. 1.
Change in SBP from baseline to week 26
(mmHg)
Patient group
Liragutide
1.8 mg Placebo
Difference
between
liraglutide
and
placebo
Overall
–2.55 0.19 –2.37
AH treat at week 26 –2.03 0.76 –2.79
No AH treat
–3.07 –1.13 –1.95