VOLUME 12 NUMBER 1 • JULY 2015
31
SA JOURNAL OF DIABETES & VASCULAR DISEASE
RESEARCH ARTICLE
for their regular scheduled visit to the doctor/clinic were invited
to participate in the survey. Patients who agreed to participate
provided informed written consent.
CEPHEUS was a single-visit non-interventional study. Each
patient’s record form documented patient demographics, current
LLD treatment, smoking status, known diabetesmellitus (DM), family
history of premature vascular disease, known arterial hypertension
(HT) and cardiovascular medical history. Physical examination by
the investigator was limited to measurement of height, weight,
waist circumference and blood pressure. A fasting blood sample
was drawn to evaluate the serum lipid profile [total cholesterol,
LDL-C, high-density lipoprotein cholesterol (HDL-C), triglycerides
and apolipoprotein (apo) AI and apo B], fasting blood glucose (FG)
and glycosylated haemoglobin (HbA
1c
) levels.
The primary endpoint was the percentage of patients who
achieved the LDL-C goals according to either the NCEP ATP
III/2004 updated NCEP ATP III guidelines or the fourth JETF/South
African guidelines, which were current in South Africa at the time
the CEPHEUS SA study was conducted. Secondary endpoints
included achievement of LDL-C goals in patients with and without
features of the metabolic syndrome, and primary versus secondary
prevention.
The parent study (CEPHEUS-Europe) has been registered with
the US National Institutes of Health (ClinicalTrials.gov), number
NCT00542867. The CEPHEUS study was sponsored by AstraZeneca.
The sponsor oversaw data collection and monitored study sites.
The authors had full access to the study database and all analyses
reported here were performed independently of the sponsor.
Statistical analysis
We subdivided the cohort by gender and ethnicity for the purposes
of this analysis. The four major ethnic groups in South Africa were
black Africans, Caucasians, Asians (including patients of Indian
descent) and patients with mixed ancestry. The risk category was
determined for each patient and we calculated a dichotomous
variable for each patient indicating whether their LDL-C had
reached the guideline mandated target level.
We generated descriptive statistics for all clinical and laboratory
parameters, following subdivision by gender only, and then
following subdivision by both ethnicity and gender. We analysed
the effect of ethnicity and gender on goal attainment using logistic
regression with the logit function in a model that incorporated
ethnicity and gender simultaneously.
We calculated odds ratios and 95% confidence intervals for
the probability of not attaining LDL-C goal. The probability of not
attaining LDL-C goal was referenced against Caucasian ethnicity
and male gender, for which the odds ratio was set as 1. All
p
-values
are two-sided and we regarded
p
< 0.05 as statistically significant.
All analyses were performed with Statistica [StatSoft Inc (2011),
STATISTICA (data analysis software system) version 10, www.
statsoft.com].
Results
A total of 3 001 patients consented to participate in the survey. Full
data sets were available from 2 996 patients and form the basis
of this report. About two-thirds of patients were recruited from
the private healthcare sector, with the remaining one-third coming
from public sector institutions.
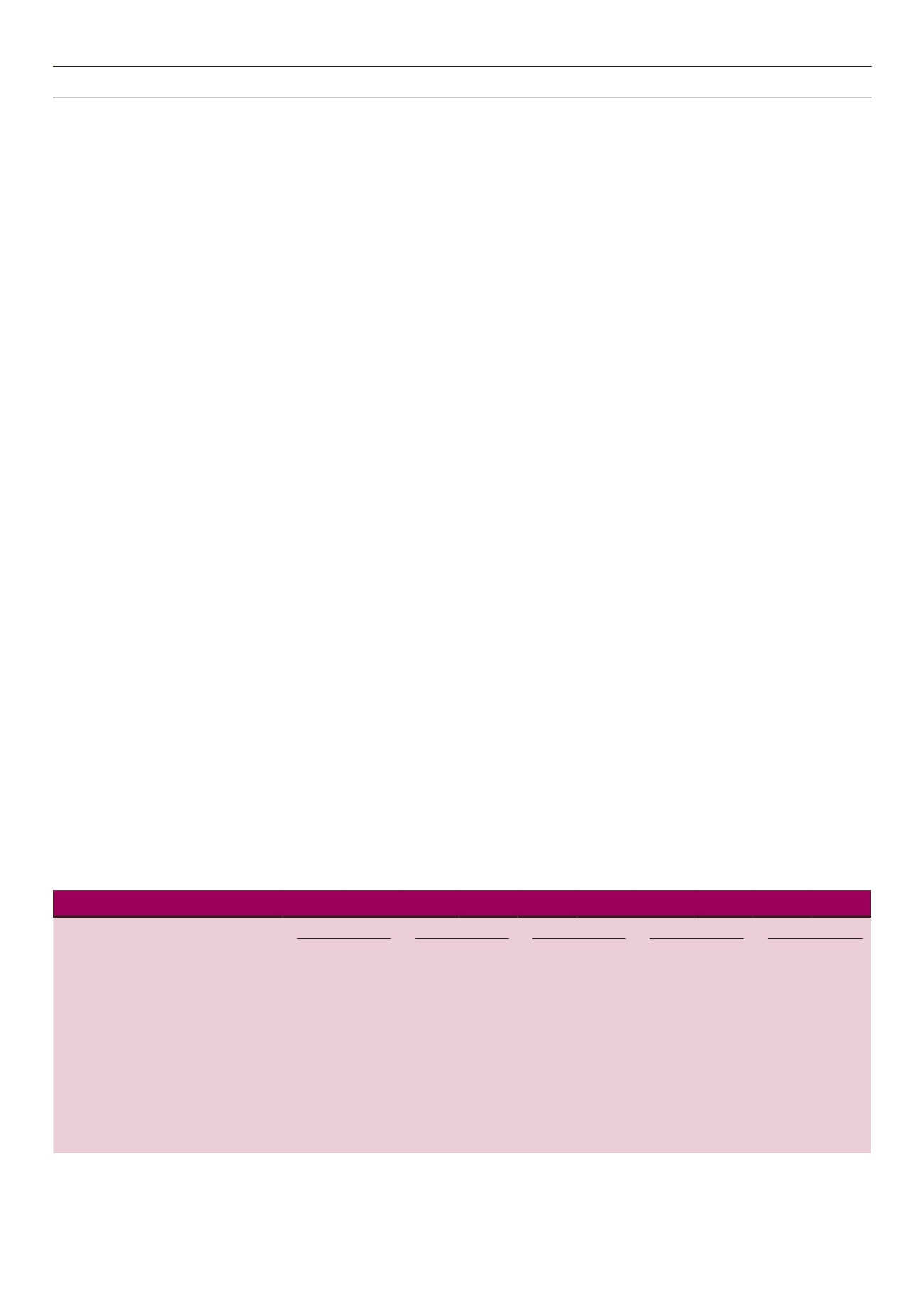
Demographic, anthropometric and clinical data are shown in
Table 1. Of the total group, 47.1% had known DM but 2.4% of
patients who did not give a history of DM had FG levels that would
qualify for the diagnosis of DM. Glycaemic control in patients who
gave a history of DM was generally poor, with a mean HbA
1c
level
of 8.33%.
The prevalence of a history of HT in this study was 71.6%. The
mean systolic blood pressure in the entire study cohort was 133.2
mmHg, with a diastolic pressure of 80.2 mmHg. In those subjects
with a history of HT (Table 2), the mean systolic blood pressure was
136.1 mmHg, with a diastolic pressure of 81.3 mmHg. African-
ancestry males had the highest systolic blood pressure and females
of mixed ancestry the highest diastolic blood pressure but the inter-
ethnic differences were small.
More Caucasian patients were receiving LLDs for primary
prevention compared to those of African ancestry, few of whom
were on treatment for primary prevention. The majority were
receiving treatment for the CVD risk equivalent of DM.
The percentage of African patients who were on LLDs for coronary
artery disease (CAD) was lower than that seen in the other ethnic
groups. The prevalence of CAD was higher in males than in females
in all ethnic groups. Among male participants, CAD rates were
highest in men of Caucasian, Asian and mixed ancestry. Among the
women, the highest prevalence of CAD was in women of mixed and
Asian ancestry. Few African patients gave a family history of CAD
and the percentage of smokers was also lowest among the African
patients. Most patients (95.9%) were on LLD monotherapy, with this
being almost exclusively (98.9%) statin based.
Table 1.
Baseline characteristics
Entire study
Caucasian
African
Mixed ancestry
Asian
Characteristics
Male Female Male Female Male Female Male Female Male Female
Number
1572
1424
818
567
168
342
222
259
364
256
Mean age (years)
59.2
59.6
60.9
62.0
57.4
57.4
58.1
59.0
56.8
58.0
Current smoker (%)
18.6
10.8
15.9
14.3
15.6
2.6
25.1
19.7
21.4
5.1
Family history of vascular disease (%)
27.0
29.5
29.0
36.3
4.1
11.1
25.2
30.9
39.2
37.5
Mean body mass index (kg/m
2
)
29.2
30.8
30.0
29.4
29.3
34.2
29.0
31.2
27.6
29.4
Mean waist circumference (cm)
101.0 101.0 105.7
95.6
101.5 102.2 101.7 100.4
99.4
97.6
Known diabetes mellitus (%)
45.8
48.5
34.4
26.8
70.6
74.9
54.1
54.5
38.7
55.1
Known systemic hypertension (%)
68.8
74.6
64.7
64.7
84.6
88.9
76.6
84.2
65.8
67.9
History of coronary heart disease (%)
45.8
23.9
46.3
19.6
19.0
14.3
58.1
38.2
49.4
31.6
History of cerebrovascular disease (%)
5.8
4.8
5.3
4.4
5.9
6.1
6.3
4.2
6.3
4.2
History of peripheral arterial disease (%)
6.2
3.5
7.8
3.2
3.0
2.6
6.8
6.2
3.3
2.7



















