RESEARCH ARTICLE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
78
VOLUME 13 NUMBER 2 • DECEMBER 2016
isonitrile (99mTc-MIBI), the patients were given one to two tablets
of sublingual nitroglycerin (0.4 mg), five minutes apart and they
were injected with 740 MBq (20 mCi) of MIBI. A GSPECT study was
performed 45 minutes later.
GSPECT data were acquired in the supine position with the
double-head SPECT-
γ
camera equipped with a high-resolution low-
energy collimator. The obtained data were projected as myocardial
tomographic slices in short-axis, vertical long-axis and horizontal
long-axis views. Electrocardiogram gating was applied to the
cardiac cycle with eight frames per cardiac cycle. The myocardium
was divided into 17 segments following the American Society
of Nuclear Cardiology/American College of Cardiology/American
Heart Association guidelines.
8
GSPECT dates were processed and analysed using 4D-MSPECT
software, which determines the extent and severity of left ventricular
perfusion defect size and the extent of reversible (ischaemia) or fixed
(scar) perfusion defects.
9
The programme assigned a score of 0 to 4
to each segment based on activity level: 0 = normal, 1 = equivocal,
2 = moderate, 3 = severe reduction of radioisotope uptake, and 4 =
absence of detectable tracer uptake. Abnormal perfusion, motion
and thickening were defined as a score of ≥ 2.
The summed stress score (SSS), summed rest score (SRS), and
summed difference score (SDS) were calculated based on the
conventional 17-segment model. The summed difference score
(SDS), indicating the extent of reversible perfusion defects, was
obtained by calculating the differences between the SSS and SRS.
Statistical analysis
Statistical analyses were performed using SPSS 18.0 software.
Parametric values are given as mean ± standard deviation and
non-parametric values as a percentage. To compare parametric
continuous variables, the Student’s
t
-test was used; to compare
non-parametric continuous variables, the Mann-Whitney
U
-test was
used. Categorical data were compared by chi-square distribution.
Stepwise multivariate logistic regression models were created to
determine independent variables for myocardial perfusion defect.
For multivariate regression, variables with a
p
-value < 0.1 in
univariate analysis were selected. Two-tailed
p
-values < 0.05 were
considered to indicate statistical significance.
Results
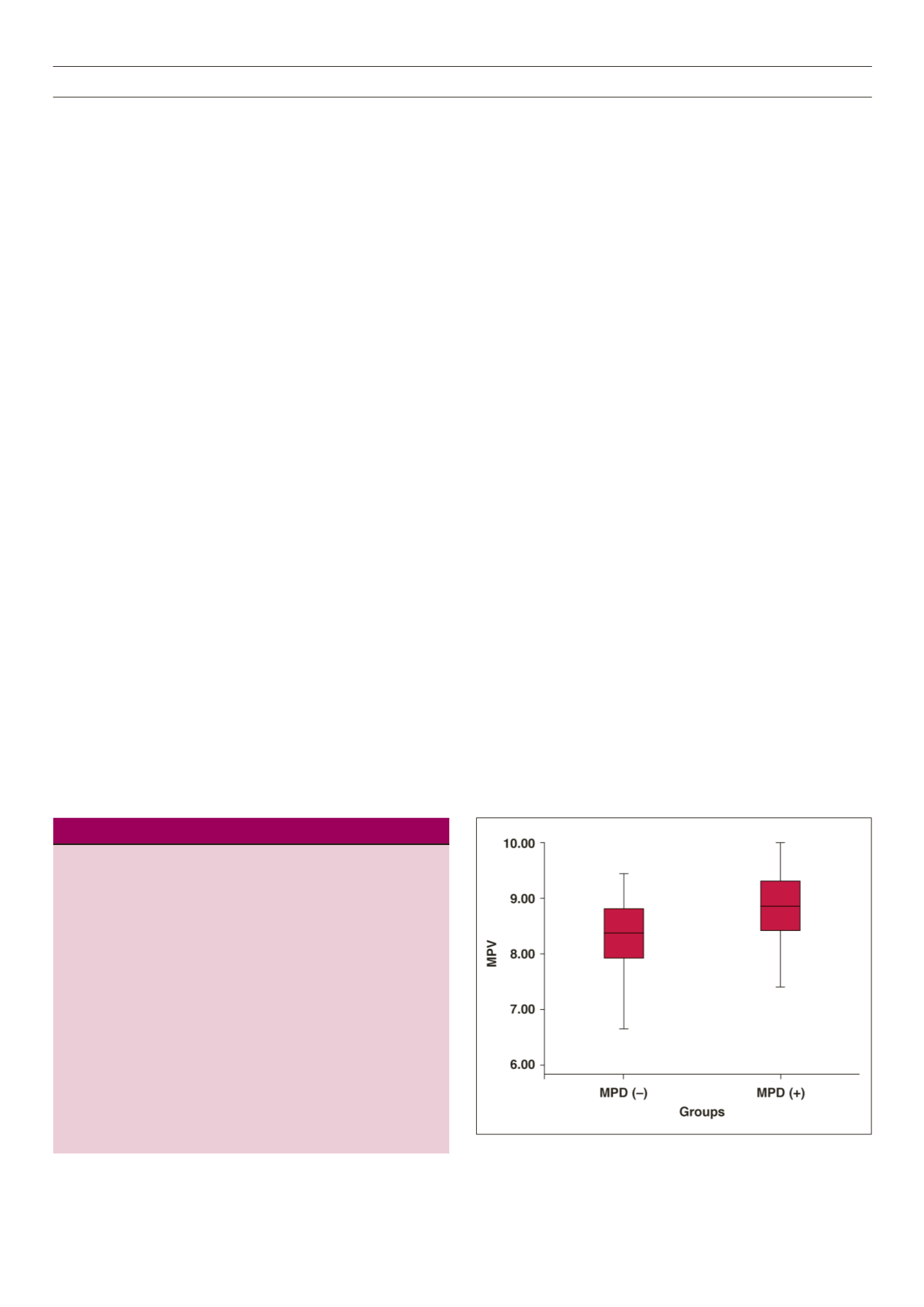
Baseline characteristic of the patients are given in Table 1. Levels
of glucose, triglycerides (TG), total cholesterol (TC), low-density
lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL)
cholesterol, haemoglobin (Hb) and glycosylated haemoglobin
(HbA
1c
), and body mass index (BMI) in the two groups were not
statistically significantly different. The MPV level was higher in
group 1 than in group 2 patients (8.76 ± 0.78 and 8.25 ± 0.78
fl, respectively,
p
= 0.003). Levels of MPV in the two groups are
shown in Fig. 1.
Univariate analysis showed that MPV, and HbA
1c
and glucose
levels were significantly involved in myocardial perfusion defects.
Multivariate logistic regression analyses showed that MPV was the
only variable independently associated with myocardial perfusion
defect (OR: 2.401, 95% CI: 1.298-4.440,
p
= 0.013) (Table 2).
Discussion
This study showed that there was a relationship between myocardial
perfusion defect and MPV. MPV was higher in the group with
myocardial perfusion defects, compared to the one without
myocardial perfusion defects. Patients with diabetes develop
vascular complications, including macrovascular complications
[coronary artery disease (CAD), peripheral vascular disease and
stroke] andmicrovascular complications [diabetic nephropathy (DN),
diabetic retinopathy (DR) and peripheral neuropathy].
10
Continuous
hyperglycaemia may cause endothelial dysfunction and vascular
lesions, resulting in diabetic vascular complications.
11,12
Type 2 diabetes is a substantial risk factor in atherosclerotic
cardiovascular disease.
13,14
Cardiovascular disease (CVD) is the
leading cause of death in patients with type 2 DM.
15
Asymptomatic
CAD is common in patients with DM and is a strong predictor of
future poor outcome of coronary vascular events, as well as early
death.
16,17
DM is associated with generalised endothelial dysfunction
and small-vessel abnormalities.
18,19
Perfusion defects are substantial predictors of coronary events in
patients with known or suspected coronary heart disease (CHD).20
It is proposed that concomitant abnormalities of perfusion imaging
scans in patients with diabetes with normal coronary angiograms
Table 1.
Baseline characteristic of the patients.
Group 1
Group 2
p
–value
Age (years)
60.02 ± 9.28
60.81 ± 8.02
0.660
Women (%)
72.7
68.2
0.408
HT (%)
72.7
86.4
0.093
HL (%)
47.7
56.8
0.281
Aspirin (%)
34.1
29.5
0.410
BMI (kg/m
2
)
31.41 ± 6.23
30.41 ± 5.7
0.446
Glucose (mg/dl)
131.79 ± 40.553
151.16 ± 54.213
0.070
TG (mg/dl)
192.36 ± 116.48
171.71 ± 87.321
0.600
TC (mg/dl)
190.04 ± 42.25
178.83 ± 46.73
0.258
HDL-C (mg/dl)
40.58 ± 5.911
38.68 ± 6.08
0.167
LDL-C (mg/dl)
118.77 ± 28.75
108.28 ± 33.82
0.133
Hb (g/dl)
13.16 ± 1.40
13.42 ± 1.46
0.399
MPV (fl)
8.76 ± 0.76
8.25 ± 0.78
0.003
HbA
1c
(%)
8.67 ± 0.68
8.35 ± 0.86
0.094
HT: hypertension; HL: hyperlipidaemia TG: triglycerides; TC: total
cholesterol; HDL-C: high-density lipoprotein cholesterol; LDL-C: lowdensity
lipoprotein cholesterol; Hb: haemoglobin; MPV: mean platelet
volume; HbA
1c
: glycosylated haemoglobin.
Fig. 1.
MPV levels in the two groups.



















