VOLUME 14 NUMBER 1 • JULY 2017
9
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
of endothelial cells and fibroblasts, accelerating the development
of granulation tissue over which epidermal cells migrate and so
enhance wound healing.
37
Despite the fact that LLLT is not an established treatment
modality for ulceration in South Africa, a number of studies, case
reports and clinical trials with humans have shown good ulcer
healing outcomes using LLLT. Beckmann and colleagues conducted
a systemic review in 2014 of the relevant literature on LLLT for the
treatment of DFUs and found that several clinical studies had been
published between 1998 and 2011, suggesting that LLLT promotes
wound healing of diabetic ulceration.
12
A summary of these clinical
trials is presented in Table 2.
such as methicillin-resistant
Staphylococcus aureus
(MRSA),
Propionibacterium acne
and
Pseudomonas aeruginosa
.
16
Enwemeka
et al.
found that blue light (470 nm) was able to kill MRSA
in vitro
.
44
Lipovsky
et al
. suggested that high-intensity visible light in the
range of 400–1 000 nm is bactericidal to
S aureus
,
P aeruginosa
and
Escherichia coli
, to name a few.
45
Irradiation at a wavelength of
408nm was proposed by Ankri and colleagues in treating infected
wounds to clear an infection, followed by irradiation at 730nm to
speed up the healing process.
43
According to the literature, red as well as blue light lasers improve
perfusion by releasing nitric oxide (NO) from nitrosyl complexes
with haemoglobin, enhanced epithelialisation and elevated
keratin-10 mRNA levels.
38
It has been discovered that the activity
of cytochrome c oxidase is inhibited by NO and this was initially
seen as an imperfection.
36
However blue light also facilitates the
recovery of mitochondria inhibited by NO gas by releasing NO from
the mitochondrial complexes. Therefore improved wound healing
via the NO pathway induces endothelial cell migration by activating
growth factors, resulting in an increase in keratin expression.
38
This
shows that a combination of red and blue light lasers can be used
to treat infection to promote and enhance the healing process of
infected DFUs, since infection plays a role in delaying the wound
healing process.
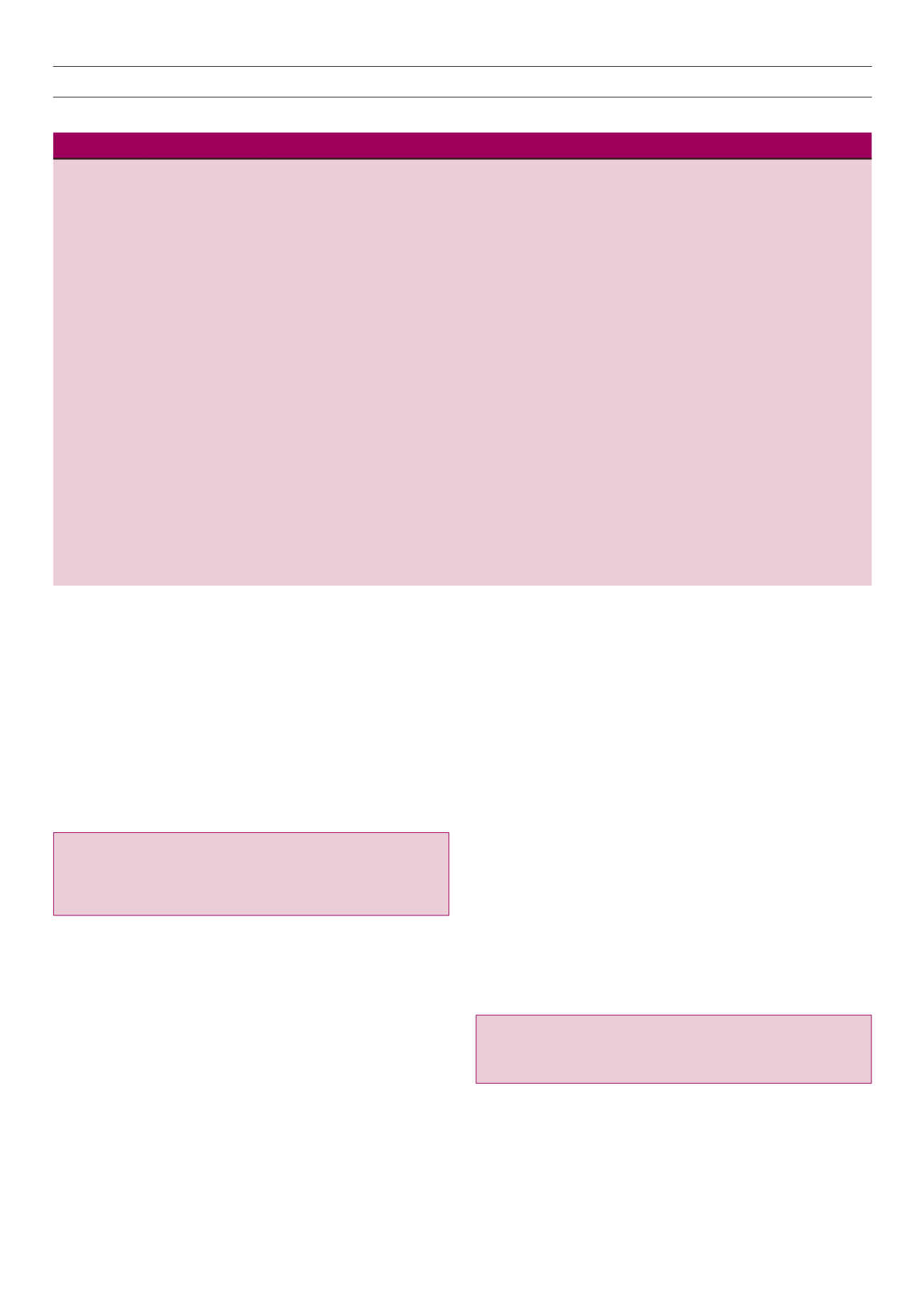
Table 2.
Clinical trials on lower-limb ulcer treatment with LLT in diabetic ulcers
Study
Study design
Participants
Intervention
Outcome
Kazemi-Khoo
(2006)
Prospective
cohort study
7 type 2 diabetes
patients with grades
2 and 3 diabetic foot
ulcers
Red light (660 nm; power: 25 MW; 0.6–1 J/cm
2
)
and ulcer margins with infra-red laser (980
nm; power: 200 MW; 4–6 J/cm
2
) along with
intravenous laser irradiation with red light laser
(650 nm; power: 1.5 MW) for 15–20 min, in
addition to laser acupuncture with infrared laser
(1 J/cm
2
). Sessions were every other day for 10–15
sessions (route 1) and then continuing the course
twice weekly (route 2) until complete recovery
was achieved
Complete recovery was achieved in
all cases and there was no relapse
after an average of about 19
sessions. Only 1 case took a total of
26 sessions (route 1).
Minatel
et al
.
(2009)
Randomised,
placebo-controlled,
double-blinded
trial
14 patients with 23
chronic diabetic ulcers
LLLT: 660nm and 890nm, 3J/cm
2
, 30sec/5cm
2
twice a week for 90 days/until healed
LLLT group had more granulation
(day 30: 56%) and faster healing
(day 30: 79.2%), 58.3% healed fully
(1 ulcer placebo group); 75% ulcer
healed 90–100% day 90 (1 ulcer
placebo group)
Mokmeli
et al.
(2010)
Prospective
cohort study
74 DFUs
LLLT: 650 nm and 860-nm laser, with total
energy density of 3.6 J/cm² plus intravenous laser
therapy (IVL) with 2.5-MW, 650-nm laser used for
30 minutes
Excluding the wounds that were
found to be in stage 5, more than
80% of each categorised stage
were found to have been almost
completely healed (by more than
50%) within a 2-month period
Kajagar
et al.
(2012)
Randomised
controlled trial
68
patients
with
chronic DFUs (grade 1)
Daily treatment for 15 days, 2–4-J/cm
2
power,
60-mW frequency, 5kHz
Significant reduction of percentage
of ulcer area in the LLLT group
Key message:
Phototherapy can enhance wound healing of
DFUs, since it exhibits bactericidal effects as well as stimulating
cellular repair and growth.
Conclusion
Diabetic foot ulceration still proves to be a difficult condition to
manage and generally has a negative impact on the patient’s
Key message:
Once acute inflammation has been induced in
DFUs by mechanical or sharp debridement, the healing process
can be further promoted by LLLT, which stimulates cellular
proliferation and wound healing.
Phototherapy, bactericidal effects and cellular repair enhance
wound healing
Various wavelengths are used for different applications in
phototherapy as they have different depths of penetration into
human tissue. Visible red, infra-red and near infra-red have
been demonstrated to penetrate deep tissue and are absorbed
by cytochrome c oxidase, compared to violet and blue spectrum
lasers.
39,43
When blue laser light is absorbed by flavins (flavoproteins)
and porphyrins that lack transition metal coordinating, these
molecules have been shown to have bactericidal effects through the
production of reactive free radicals, which destroy bacteria.
35,37-39
A number of studies have found that, at different wavelengths,
blue light laser is bactericidal to different infectious organisms,



















