VOLUME 14 NUMBER 1 • JULY 2017
7
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
Similarly, in a study conducted by Faglia
et al.
over a 90-day
period where the efficacy of RCW and a non-removable fibreglass
off-bearing cast (TCC) were compared in DFU healing, it was
reported that 73.9% of patients in the TCC group and 72.7% in
the RCW group achieved complete healing.
28
Overall, these studies
show that whether the off-loading device is removable or non-
removable, it can be used effectively to redistribute pressure on the
plantar aspect of the foot. However results are dependent on the
patient’s compliance to constantly wear removable devices.
results were observed; ulcers showed a 6-cm
2
reduction within
the mean ulcer surface area (MSA) versus a 1-cm
2
reduction in
the control group. However, it was noted that the reduction in
MSA between the study groups over the entire period was not
statistically significant. Nevertheless, wounds after debridement
alone are capable of regressing in 57% of the days between visits
because there is balance shift favouring the biofilm, even though
the rate of healing immediately after debridement is more rapid.
32
It has been suggested that frequent debridement of DFUs and
chronic venous leg ulcers, as part of wound treatment, may increase
wound healing rates and closure of the ulcer.
33
If debridement is
done in a sequential fashion, it will avoid the re-establishment
of microbial biofilm growth and tissue devitalisation, which is
responsible for delayed healing of ulcers.
7,32
Wilcox and colleagues investigated the frequency of debridement
and the time to heal for different types of ulcers, including DFUs
and chronic venous ulcers. This study noted that the median time
to heal after weekly or more frequent debridement for DFU was 21
days, compared to 64 days when debridement frequency was in the
range of every one to two weeks, and 76 days when debridement
was once every two weeks or more.
34
Furthermore, in a study performed by Ahmad and colleagues,
which assessed the efficacy of radical debridement and skin
grafting in treating DFUs, compared with other conservative wound
treatments (such as the use of dressings, negative-pressure wound
therapy and hyperbaric oxygen), the results showed a 100%
skin graft take in 80% of the patients on day four after surgery.
Debridement in this study was performed three times a week, every
second day, and the amount of granulation tissue was assessed
before skin grafting. The mean healing time and hospital stay was
lower in the skin-graft group compared to the control group (4.0 ±
1.5 vs 10.0 ± 1.0 weeks).
31
These findings suggest that aggressive
and repeated debridement definitely does increase ulcer healing
rates of chronic wounds.
Both off-loading and debridement methods are regularly
practised by podiatrists to promote the healing process of diabetic
lower-limb ulcers. Additionally, selecting the right type of wound
dressing is also important to aid the healing process, and this is
also dependant on the characteristics of the individual ulcer that is
receiving treatment.
9,13,14,19
Debridement practises offer an opportunity for additional
antibiotic interventions, applied topically and/or systemically, which
temporarily disrupt biofilm defence colonies, forcing microbes to
become more susceptible to these interventional treatments as
well as the host’s immune defenses.
32
A summary of these clinical
studies is presented in Table 1.
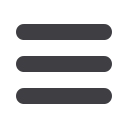
Key message:
Total-contact casting has been shown to be
effective in redistributing pressure in the plantar aspect of the
foot and so either prevents ulcers from re-occurring or promotes
healing of current DFUs.
Fig. 5.
Total contact cast.
Key message:
Mechanical or sharp debridement is one of the
essential treatment procedures in podiatry with which chronic
inflammation can be converted to acute inflammation to
promote DFU healing.
Wound debridement
In wound-healing clinics, various types of debridement techniques
can be used by podiatrists to treat DFUs, such as surgical and sharp
debridement, mechanical, autolytic and enzymatic debridement,
and larval debridement.
29
Debridement is the most important step
towards achieving chronic diabetic wound healing, as it transforms
chronic wounds into acute wounds.
30
Unlike acute wounds, chronic diabetic ulcers seldom follow
the normal pattern of repair due to various physiological factors
such as hypoxia, dysfunction in the fibroblasts and epidermal
cells, impaired angiogenesis and neovascularisation, high levels
of metalloproteases, damage from oxygen radicals and advanced
glycation end-products, which delay wound healing.
7,31
In addition,
there is also sometimes an accumulation of non-viable tissue
(calluses) and slough with excess exudate, which also encourages
bacterial colonisation (biofilm), promoting the risk of infection and
so preventing healing.
31,32
Sharp debridement (scalpel debridement) helps to break down
bacterial colonies, thus reducing the bacterial load of an ulcer even
in the absence of overt infection, and so promotes the release of
growth factors to aid the healing process.
32
When combined with
standard or advanced therapies that are currently used in ulcer
treatment, the net rate of healing is increased.
32
Williams and colleagues evaluated the effect of sharp
debridement on the progression of recalcitrant chronic venous leg
ulcers. This study concluded that sharp debridement was effective in
stimulating the healing of ulcers. It was conducted over a 12-month
period and already at four weeks post-debridement, some positive
Phototherapy
Phototherapy is a therapeutic modality that involves the application
of laser light, at a particular wavelength and at low intensities, to
tissue to stimulate various biological processes.
16,35
Low-level laser
therapy (LLLT) is widely used to accelerate tissue repair in surgery,
dentistry, dermatology, somatology, pain management and ulcer



















