80
VOLUME 15 NUMBER 2 • NOVEMBER 2018
PASCAR ROADMAP
SA JOURNAL OF DIABETES & VASCULAR DISEASE
importance of reaching minimum standards (Table 3) for the health
systems of countries to achieve the 25% hypertension control
target. Implementation of these solutions and suggestions on
customising the overall strategy at a country level are discussed.
The WHF roadmap provides a general framework that could
be useful for LMICs, however, to be implemented it should
be customised according to the local context. With PASCAR’s
leadership and the contribution of other professional organisations,
this approach seems to be at the right time to turn the many
hypertension challenges in Africa into immense opportunities.
Although population-based strategies for lowering BP may be cost-
effective, they are not the focus of this roadmap, but we recognise
these would be beneficial.
Methods
In January 2014, panel members who were appointed to develop
the PASCAR roadmap were invited to join the PASCAR task
force on hypertension. Based on their expertise and leadership
in hypertension, 41 nominees from 21 countries received
invitations, with 95% responding positively. These experts included
cardiologists, nephrologists, public health physicians, researchers
(including clinical trialists), nurses, pharmacologists, evidence-based
medicine specialists and guideline developers.
During the first face-to-face meeting held in Nairobi on 27
October 2014,
14
the group acknowledged the lack of a continental
strategy to address the hypertension crisis. A decision was taken
to develop a roadmap for the prevention and management of
hypertension in Africa as a matter of urgency under the auspices
of the WHF.
To customise the WHF BP roadmap for Africa, the core group
performed a comprehensive literature search and communicated
with the WHF from November 2014 to July 2015 via teleconference
and e-mail. After receiving and comprehending the WHF roadmap
document, task force members held a second face-to-face meeting
in London on 30 August 2015, to make suggestions on its relevance
and customisation. A detailed presentation of this roadmap
was reviewed and discussed by PASCAR task force members,
hypertension experts and leaders of hypertension societies via
e-mail, with WHF feedback.
Development of a warehouse for African guidelines and clinical
trials on hypertension was also reviewed. Finally, the steps in
developing the African roadmap for reducing CVD mortality rates
through BP control was planned.
The first draft of the PASCAR roadmap for hypertension
management and control was presented in Mauritius on 4 October
2015. Attendees were 13 presidents of national cardiac societies
or representatives, the president of the International Forum for
HypertensionControl andCardiovascularDiseasePrevention inAfrica
and representative of the International Society of Hypertension,
a representative of the African Heart Network, members of the
PASCAR task force on hypertension, and scientists from the WHF.
The draft was reviewed and oral and e-mail comments were received
from participants. The WHO PEN programme
12
was compared with
the PASCAR hypertension roadmap to ensure complementarity
between the two documents.
The second version of the roadmap draft was submitted to a
core group for internal review from October to December 2015.
In March 2016, a selected group of hypertension experts from 12
French-speaking countries met in Yaoundé to discuss the algorithm
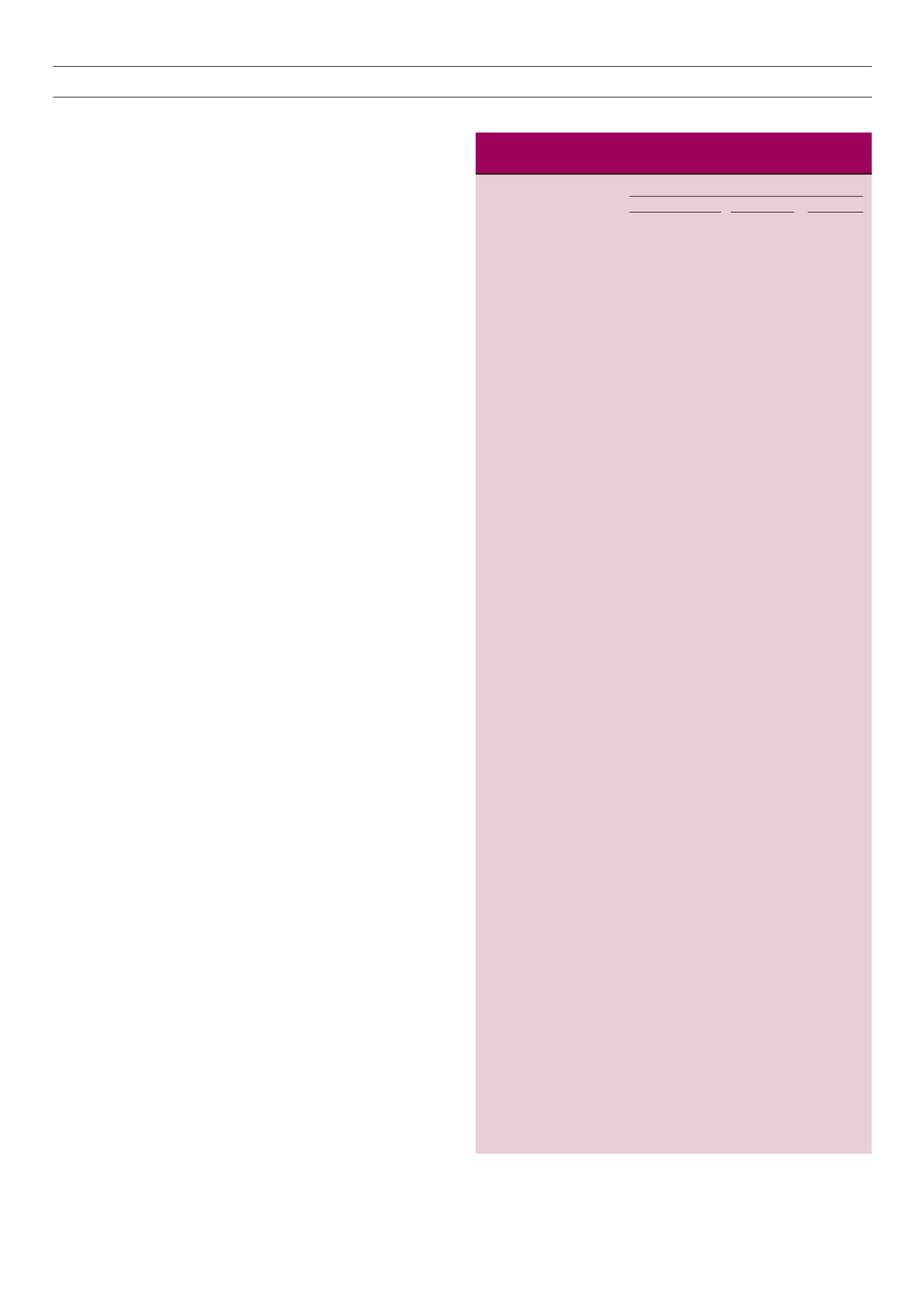
Table 3.
Minimum care for hypertension management at each healthcare
level in Africa
Level of care
Primary
Secondary
Tertiary
Basic staff, equipment,
Trained health Medical
test and medication
worker or nurse Practitioner Specialist
Basic equipment
Automated blood pressure
+++
+++
+++
devices, or calibrated
sphygmomanometer, either
mercury or oscillometric
plus appropriate cuffs
Home blood pressure
+
+++
devices
Ambulatory blood
+/–
+++
pressure devices
Tape measure for waist
+++
+++
+++
circumference
Scale for weight
+++
+++
+++
Stadiometer for height
+++
+++
+++
Standard 12-lead ECG
++
+++
Glucometer
+
+++
+++
Funduscope
++
+++
Stethoscope
+++
+++
+++
Basic tests
Urine dipsticks for
+++
+++
+++
protein, blood and glucose
Standard 12-lead ECG
++
+++
recording
Glucometer strips for
testing glucose + +++ +++
Na+, K+ and creatinine
+
++
+++
with calculation of eGFR
Cholesterol
+
+++
Glycated haemoglobin
+
++
+++
(HbA
1c
)
Chest radiograph
+/–
+++
Basic medication classes with examples*
Thiazide or thiazide-like
+++
+++
+++
diuretic (hydrochlorothiazide,
indapamide,
chlorthalidone)
Calcium channel blockers
+++
+++
+++
(amlodipine, nicardipine,
long-acting nifedipine)
Angiotensin converting
+
+++
+++
enzyme inhibitor
(enalapril, lisinopril,
perindopril, ramipril)
Angiotensin receptor
+++
+++
blockers (candesartan,
valsartan, losartan)
Vasodilating beta-blockers
+++
+++
(nebivolol, bisoprolol,
carvedilol)
Spironolactone
+++
+++
Long-acting
α
-blocker
+
+
(doxazocin)
Combinations of blood
+
+++
+++
pressure-lowering
medications
+++: strongly recommended; ++ moderately recommended, +:
recommended; –: not done; +/–: done if facilities are available.
*Availability of drugs at each level of care has been indicated and
recommended here for initiation only, all drugs can be used once initiated by
a medical practitioner.
A trained healthcare worker may initiate and follow up some medication.



















