VOLUME 10 NUMBER 1 • MARCH 2013
5
SA JOURNAL OF DIABETES & VASCULAR DISEASE
FUNDING DIABETES CARE
affordability and sustainability of the Discovery Health Medical
Scheme. The Scheme must be sustainable and provide our members
with peace of mind that they will be covered when they need it.
We understand the importance of managing chronic diseases
of lifestyle through co-ordinated chronic care management and
offer our members full cover for diabetes. Discovery Health has a
comprehensive, flexible and holistic approach to providing cover for
medicines for chronic diseases across the board. This approach is
fully compliant with the prescribed minimum benefits and all other
applicable aspects of the Medical Schemes Act.
The prescribed minimum benefits state that all medical schemes
are by law obliged to cover costs related to the diagnosis, treatment
and care of any life-threatening emergency medical conditions, as
defined in the Medical Schemes Act of 1998. This set of conditions
includes 270 defined diagnoses, their associated treatments and
27 chronic conditions, including type 1 and 2 diabetes mellitus.
Patients who have been diagnosed with type 2 diabetes are also
eligible for the funding of treatment with lipid-lowering drugs.
To manage these funding challenges, Discovery Health funds
all chronic medications for chronic diseases through the CIB.
Members who want to register on the CIB need to ask their doctor
to complete an application form, which includes the clinical entry
criteria requirements for them to be accepted on the benefit. Each
chronic condition has clinical entry criteria and if a member does
not meet these criteria, he/she will be unable to access the CIB for
this particular medicine.
We offer our members extensive and flexible cover for approved
chronic medicine. Members on the CIB have two options when it
comes to selecting their medicine. They can either select and claim
for medicine that is included on the formulary and which Discovery
Health will pay in full, or they can choose to use a medicine that is
not on the list, for which Discovery Health will pay the chronic drug
amount for that medicine. If the medicine costs more, members
may need to make a co-payment.
Through the CIB, Discovery Health provides members with
comprehensive, holistic care and management for their chronic
diseases. Discovery Health has added specific benefits to assist
members who want to access additional cover. Discovery Health
Medical Scheme provides members on the top-end Executive and
Comprehensive health plans access to the Specialised Medicine
and Technology benefit, which provides them with additional
cover for certain innovative medical technologies and expensive
medicines. Members who require access to medication that is not
on the formulary can request that their case be considered on
appeal, through which a doctor can demonstrate and motivate
why the member should be allowed to access the required
medication and be covered for it.
Discovery Health formulary
The Discovery Health formulary is fully compliant with the Council
of Medical Schemes’ algorithms and is designed to cater for the
patient with mild to moderate disease. Patients with a greater
severity of disease or any other complicating factors need to
go through the appeals process. Any newer drug classes which
are not currently listed on the Council of Medical Schemes’
algorithms are not included in the Discovery Health formulary.
Any member, who may, for clinical reasons, require a medicine
that cannot be covered within the Chronic Drug amount
can apply for a clinical exception, and the application will be
reviewed and assessed by a clinical team. Medicine approved
to treat conditions included in the Chronic Disease list and the
Additional Disease list, which are listed in the Discovery Health
formulary, are funded in full up to the Discovery Health medicine
rate if they are obtained from one of our network pharmacies.
Negotiating with pharmaceutical companies
to lower costs
Discovery Health continuously negotiates with pharmaceutical
companies and drug manufacturers to reduce the cost of medicine
for our members and the single exit price of medicines for South
Africa. All these formularies are reviewed by external specialists in
the relevant clinical fields and by our clinical unit twice yearly.
Approving drugs and new technologies
One of the funding challenges medical schemes experience is in
funding new medical technologies for chronic diseases, which
may improve patient outcomes in sustainable ways. Such new
technologies come with high costs, and because of these costs,
some medical schemes have made a decision not to fund the
latest treatments.
Discovery Health’s Clinical Policy Unit reviews and assesses new
technologies and determines whether they should be funded
or not. The Clinical Policy Unit has a rigorous process to assess
new technologies and new indications for current technologies,
such as drugs, devices and technology. This process includes the
evaluation of published clinical evidence, referred to as evidence-
based medicine, the financial impact on the scheme, and a health
economics analysis. The first phase of this process is the clinical
assessment, and if the clinical evidence is sufficient to support
the recommendation for funding, the process will continue to a
financial assessment of the technology, which might include a
health economics model before being approved for funding.
Centre for Diabetes and Endocrinology’s Diabetes
Management Programme
In addition to being able to access chronic medication through the
CIB, members who are registered on the CIB are able to register
on the Diabetes Management Programme, which is a nationwide
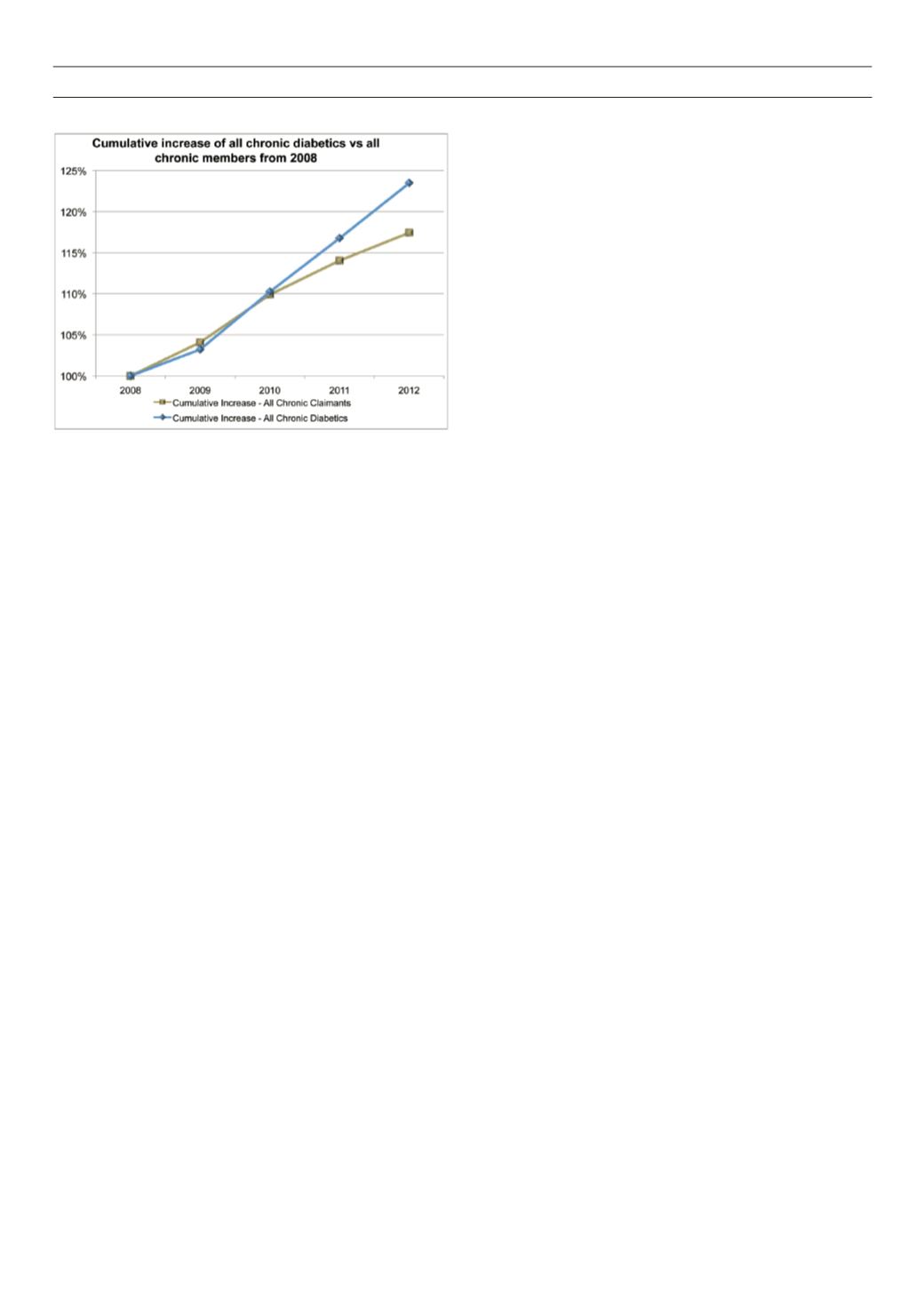
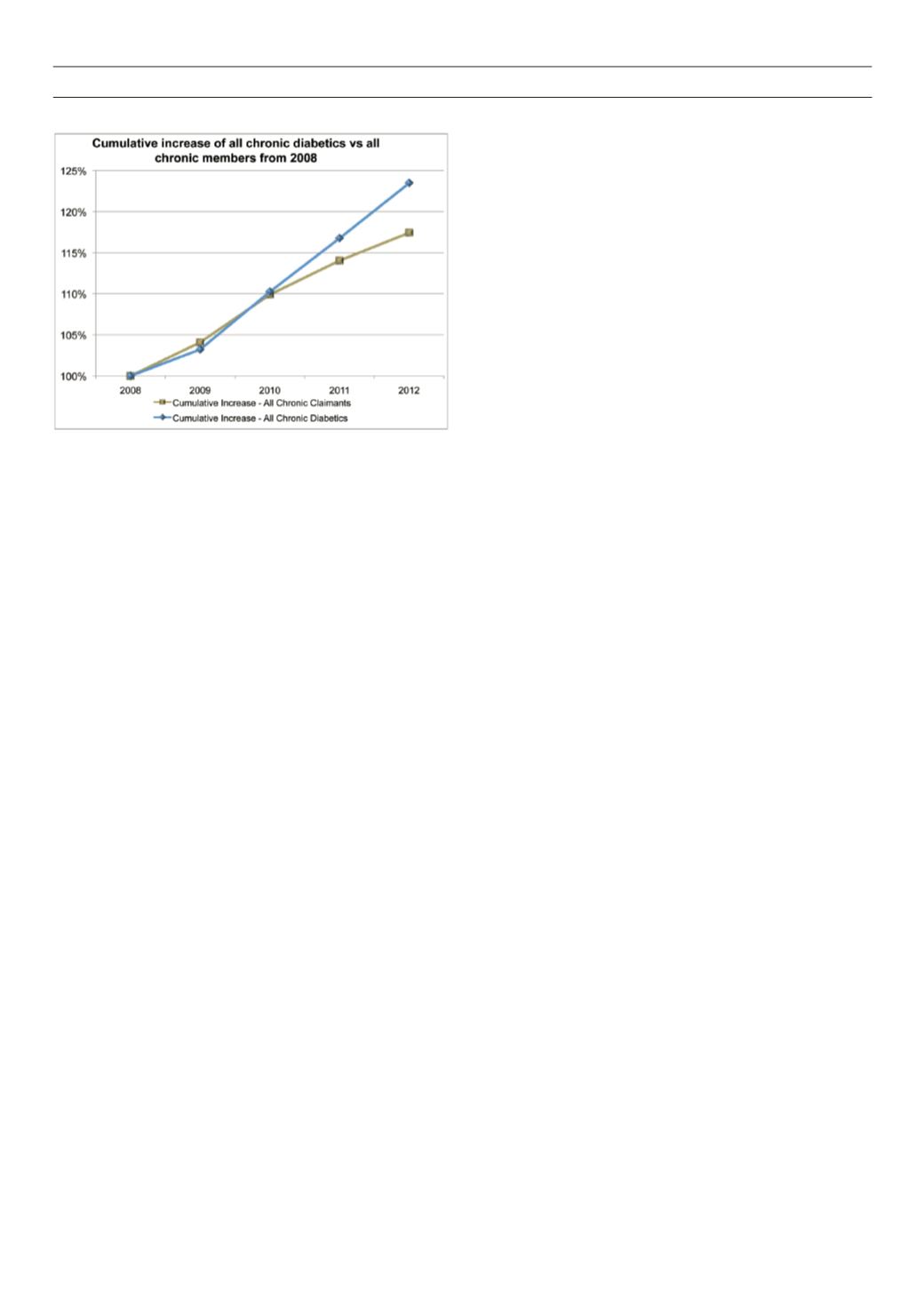
Figure 1.
Graph portraying cumulative increase of all chronic diabetics vs all
chronic members from 2008.