8
VOLUME 10 NUMBER 1 • MARCH 2013
FUNDING DIABETES CARE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
also have a good variety of anti-diabetic agents registered in South
Africa (Table 2). Physicians can therefore opt for combinations of oral
agents, or combine them with insulin or newer GLP-1 analogues.
When we treat type 2 diabetes we should all have the recently
published SEMDSA guidelines in mind,
2
as well as individualised
goals for specific patients. This will help us to select the best option
for each patient. Discussion with the patient is necessary because of
cost implications of the medication as well as individual preferences.
All patients should be on a lifestyle programme, including an
exercise routine, as well as metformin. If gastrointestinal side effects
are experienced, the glucophage XR formulation will often prevent
this. Metformin should be stopped for a week and re-challenged with
glucophage XR, starting with one tablet after supper and increasing
by one tablet every five to seven days. Two tablets are a good dose
and three are optimal. This is the easy part; from here there are many
options. I seldom use metformin in a twice-daily dosing regimen.
The best for beta-cell preservation and prevention of
hypoglycaemia is adding a GLP-1 analogue or a DDP-IV inhibitor
in early diabetes. Funders do not agree with this strategy because
it is not the cheapest. They will however often pay for insulin as a
second step, with similar cost and more risk.
The risk–benefit ratio of the thiazoledinediones is very small and
they should not be used routinely, only at the specialist level. In
the sulphonylurea class, I mainly use gliclazide MR and sometimes
glimeperide. Glibenclamide should, in my opinion, not be used
because of the much higher hypoglycaemic risk, except in the fixed
combination, Glucovance, and then only in younger patients.
The meglitinides are in a separate class, with similar effects to the
sulfonylureas but no other benefits, and are much more expensive.
I therefore seldom use them.
The DPP-4 inhibitors, whichwere recently reviewed in this journal,
are well priced and combine well with metformin.
3
They should
be used early in type 2 diabetes and always in combination. Fixed
combinations were recently launched (GalvusMet and Janumet).
These drugs have very low side-effect profiles, low hypoglycaemic
risk and are weight neutral. Multiple cardiovascular outcome trials
are currently on-going for these medications.
Triple therapy could be considered, but only if the HbA
1c
level is
close to target. The next step is insulin, usually with a basal insulin
at bedtime. One could also start with a premix with supper. Starting
dose is usually 14 to 16 units, up-titrated to achieve the specified
fasting glucose level. Titration can be done twice a week. When
the target fasting level (which should be either 6 or 7 mmol/l) is
achieved, pre-supper values should be monitored as well.
Determination of HbA
1c
levels should be repeated at this stage to
see if control has been achieved. If not controlled despite achieving
a fasting glucose level of 6 mmol/l or below, further therapy should
be added. This will require a daytime insulin, either mixed (if already
used with supper) or the basal plus short-acting insulin, and adding
short-acting analogue insulin with the main meal. Using short-
acting insulin will require more testing and patient insight, so
careful patient selection is necessary. This additional short-acting
insulin might end up as a full basal-bolus regime, always combined
with metformin.
When insulin is used twice or more a day, sulfonylureas and
DDP-4 inhibitors should be stopped. The problem is that these
patients will often require huge doses of insulin and need the
maximum tolerated dose of metfomin. The use of GLP-1 analogues
can contribute to significant insulin saving and prevention of weight
gain, which is often a problem if large doses of insulin are used.
New strategies are needed for the severely insulin-resistant
patient. The Centre for Diabetes and Endocrinology in Johannesburg
has recently studied U-500 insulin in a randomised trial, and we are
awaiting the results.
Currently we have a wide range of drugs available in this country
to fight the diabetes pandemic. Our drug availability compares well
with many European countries, however in practice, when the
clinician wants to prescribe many of these drugs, they are severely
restricted by the funders. This may be contributing to the sub-
optimal control of diabetes in this country.
References
1.
FDA website:
.
2.
Amod A, Ascott-Evans BH, Berg GI,
et al
. The 2012 SEMDSA guidelines for the
management of type 2 diabetes (Revised).
JEMDSA
2012;
17
(suppl 1): S1–S95.
3.
Lombard L. DDP-4 inhibitors (gliptins) in the management of type 2 diabetes.
S Afr J Diabetes Vasc Dis
2012;
9
(1): 10.
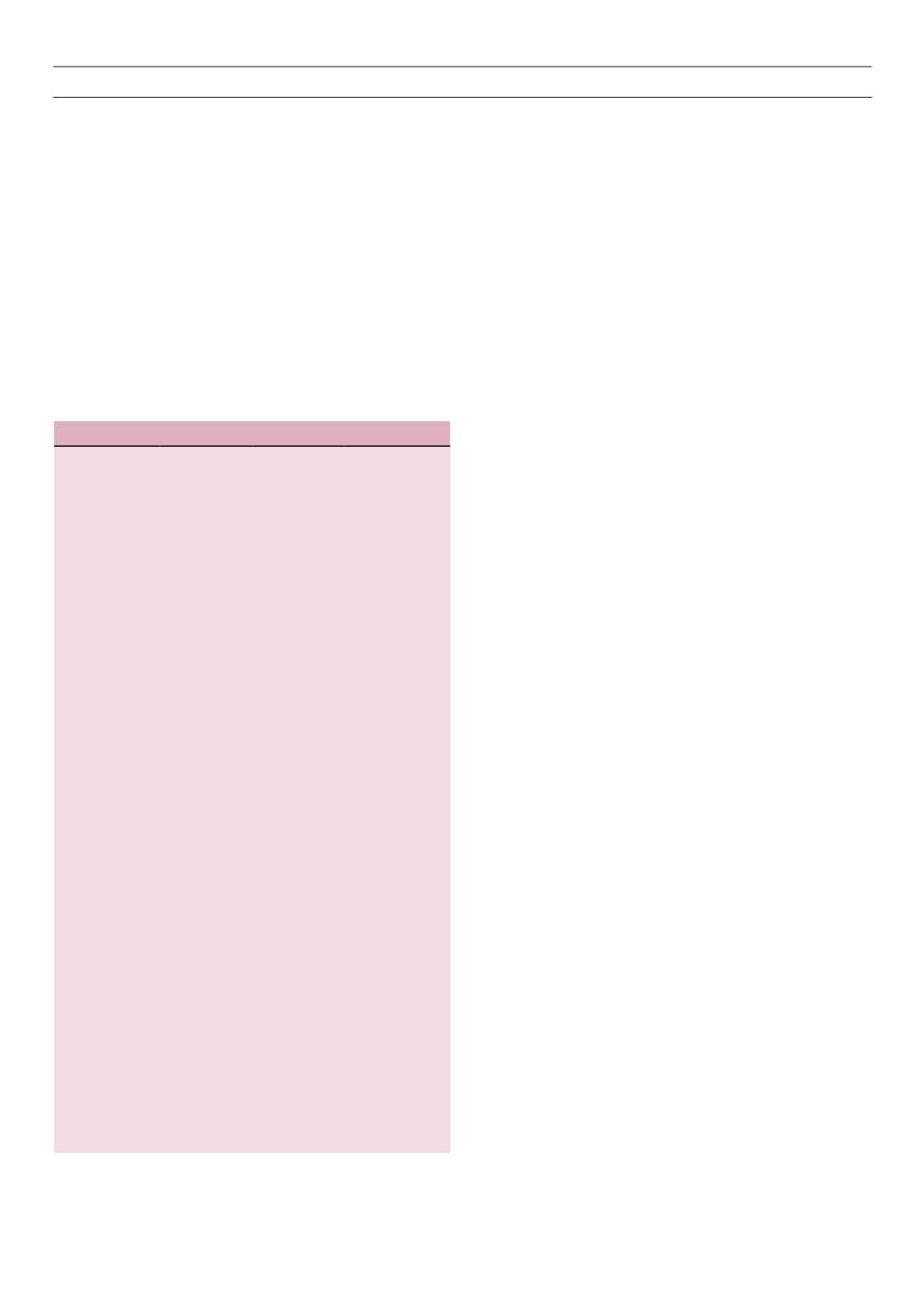
Table 2.
Registered anti-diabetic agents.
Class
Generic name *Trade name Maximun dose
Biguanides
metformin
Glucophage
3 g/day
XR 2 g/day
Sulfonylureas
gliclazide
glimepiride
glibenclamide
glipizide
Diamicron
Diamicron MR
Amaryl
Daonil
Minidiab
160 mg bid
120 mg/day
8 mg/day
7.5 mg bid
Alpha-glucosi-
dase
inhibitors
acarbose
Glucobay
200 mg tds
Meglitinides
nateglinide
repaglanide
Starlix
Novonorm
120 mg tds
4 mg qid
DPP-4 inhibitors
vildagliptin
saxagliptin
sitagliptin
Galvus
Onglyza
Januvia
50 mg bid
5 mg/day
100 mg/day
GLP-1 analogues exenatide
liraglutide
Byetta
Victoza
10 ug bid
1.8 mg/day
Thiazoledine-
diones
pioglitazone
Actos
45 mg/day
Basal insulin
Analogues
NPH
zinc insulin
detemir
glargine
Humulin N
Protaphane
Biosulin N
Biosulin L
Levemir
Lantus
unlimited
Pre-mix insulin
Actraphane
Humulin 30/70
Biosulin 30/70
Novomix-30
Humalog
mix-25 and
Mix-50
Insuman comb
unlimited
Short-acting
insulin
(analogue)
lispro
aspart
glulisine
Humalog
Novorapid
Apidra
unlimited
Human insulin
Humulin R
Biosulin R
unlimited
Combinations
Glucovance
GalvusMet
Janumet
different com-
binations and
doses
*Generic oral agents not mentioned