REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
56
VOLUME 7 NUMBER 2 • JUNE 2010
Atrial fibrillation: which patients should be managed in
primary, secondary and tertiary care?
David Jones, tom wong, diana gorog, vias markides
Definition
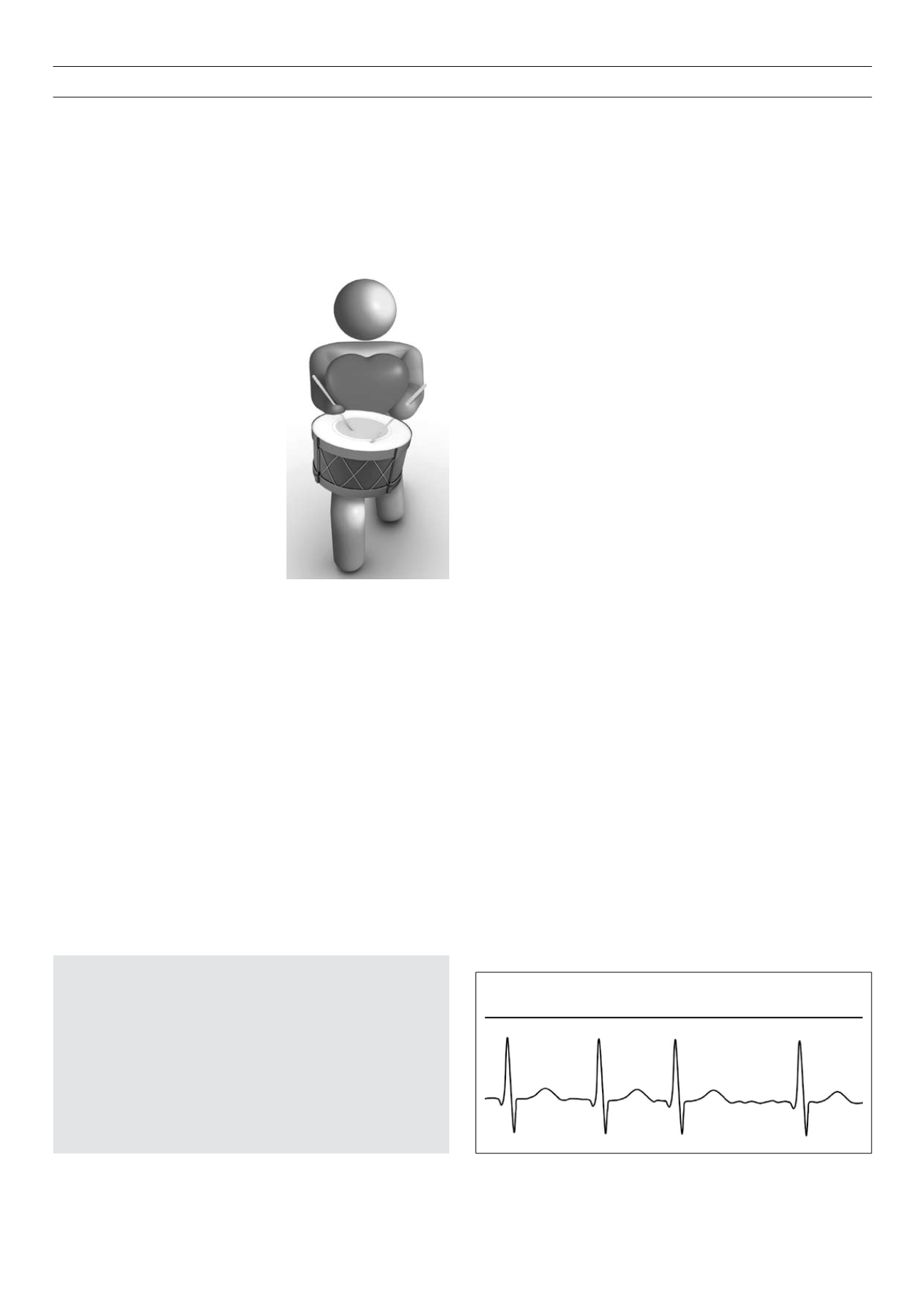
Atrial fibrillation (AF) is defined electrocardiographically as the
loss of distinct P waves
on the surface ECG accompanied by an
irregularly irregular
ventricular (QRS) response (see Fig. 1). Low
amplitude, extremely rapid and irregular (in rate and morphology)
atrial
activity may be discernible as ‘f ‘ waves. AF is usually, but not
always, associated with inappropriately rapid heart rates. It can also
be associated with significant bradycardia during sinus rhythm, and
with tachycardia during paroxysms of atrial fibrillation
(tachy-brady
syndrome)
.
Epidemiology
AF is the most common sustained cardiac arrhythmia, affecting
1–2% of the general population.
1,2
Recent studies indicate that the
lifetime risk may exceed 20%.
3
Prevalence increases with age, rising
to 8% in people over 80 years,
4
over two-thirds of individuals with
AF are aged 65–85.
5
It is estimated that there are 2.3 million people
in the United States, and 4.5 million in the European Union with
AF.
2
The prevalence is increasing – in part due to population ageing,
but also due to an increase in age-adjusted AF incidence – which
clearly has significant implications for health service planning.
AF is associated with increased mortality. In the Framingham
Study, AF conferred a relative all-cause mortality risk of 1.8.
6
Much
of this is attributable to stroke, the risk of which is increased five-
fold in those with AF – but which varies according to age and
comorbidities.
Aetiology and pathogenesis
AF is associated with several conditions, including hypertension,
heart failure and valvular heart disease, thyrotoxicosis, and
obesity.
7
Many of these conditions can cause mechanical changes
(including stretch and fibrosis) and electrical changes (remodelling)
that, when coupled with a genetic predisposition
8
and ectopic
triggers during favourable autonomic activity, can precipitate AF.
AF in itself enhances further remodelling, so encouraging its own
perpetuation.
9
The pathogenesis of AF involves a complex interplay between
mechanisms of initiation (
eg
extremely rapid electrical activity
A
trial fibrillation is the
commonest sustained
cardiac arrhythmia, and
has a significant impact on
morbidity and mortality. It is
a leading cause of stroke, and
suitable
thromboprophylaxis
should be considered in all
patients. Treatment is tailored
to the individual. This article
will review the management
strategies for patients with
atrial fibrillation, and discuss
the roles of primary, secondary,
and tertiary care.
In
Circulation of the Blood
(1628),
William Harvey commented that:
“It is … evident that the auricles pulsate, contract … and
eject the blood into the ventricles. [The auricle] has to help
infuse blood into the ventricle so that … [the ventricle] …
may send it on with greater vigour.”
This ‘primer pump’ function of the atria contributes about 10–20%
towards ventricular filling and, although not vital for normal
resting heart function, plays an increasing role in disease and in
maximising cardiac output during exercise. This function is lost in
atrial fibrillation (AF), when the atria undergo rapid and chaotic
excitation, discharging at 300–600 beats per minute.
In a normally functioning heart, the only electrical communication
to the ventricles is through the atrioventricular (AV) node, whose
electrical properties cause blockage of many of these impulses, so
protecting the ventricles from life-threatening rapidity. However,
during AF the ventricles are subjected to higher rates of excitation
than normal, particularly during exercise, and beat-to-beat variability
leads to an irregular pulse and suboptimal haemodynamics.
Furthermore, the loss of atrial contraction encourages thrombus
formation and can lead to the most feared complication of AF,
embolic stroke.
Correspondence to: David Jones
Fellow in Cardiac Electrophysiology, Royal Brompton & Harefield NHS
Foundation Trust and Imperial College London.
e-mail:
Tom Wong, consultant cardiologist, Royal Brompton & Harefield NHS
Foundation Trust and Imperial College London
Diana Gorog, consultant cardiologist, East & North Hertfordshire NHS Trust
and Imperial College London
Vias Markides, consultant cardiologist, Royal Brompton & Harefield NHS
Foundation Trust and Imperial College London
S Afr J Diabetes Vasc Dis
2010;
7
: 56–63.
doi: 10.3132/pccj.2010.001
Figure 1.
ECG in atrial fibrillation.