SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 7 NUMBER 2 • JUNE 2010
63
need to be considered in the context of patient symptoms and their
risk of stroke with non-intervention, as assessed by the CHADS2
score.
In a non-randomised comparison of medical therapy with
ablation in a general population of AF patients, ablation was
associated with improved survival, reduced symptoms, reduced
morbidity (including development of HF) and normalisation of
quality of life.
61
Several small randomised studies have compared
catheter ablation with medical therapy for maintenance of sinus
rhythm, and a meta-analysis of these has shown that ablation
results in a marked increase in freedom from AF at one year, with
an overall low level of complications comparable with other cardiac
interventions.
Ablation may also confer prognostic benefit in its ability to
restore/maintain sinus rhythm without the adverse effects of anti-
arrhythmic drugs, which themselves have never been associated
with prognostic advantage, although large prospective randomised
trials with long-term follow up are awaited – such as the ongoing
CABANA trial. Early non-randomised data suggest there is at least
a significant symptomatic and haemodynamic benefit of ablation in
patients with underlying heart failure.
64,65
Who should be referred for consideration of AF ablation?
AF is so common that catheter ablation cannot be offered to all
patients. Thankfully, most patients can be managed medically, with
appropriate reduction in thromboembolic risk and symptomatic
control (with rate or rhythm control) as the cornerstones of
treatment. However, ablation can be very useful for patients
refractory to, or intolerant of, medical treatment. Younger, highly
symptomatic patients with paroxysmal AF are obvious candidates
for the procedure as they have the highest success and lowest
complication rates, but the application of ablation techniques has
been expanded to older patients and patients with long-standing AF.
The current indication for AF ablation is symptomatic
recurrent
paroxysmal or persistent AF despite at least one class I or III anti-
arrhythmic drug
(or if these drugs are contraindicated or not
tolerated). If amiodarone is the only feasible option, then patients
would be counselled regarding the option of catheter ablation
as a ‘first-line’ rhythm control strategy, balancing the risks and
benefits of each approach. Amiodarone would be regarded as a
less favourable long-term strategy in the young.
Does catheter ablation render the patient safe to
come off warfarin?
There are, as yet, insufficient data to support a change in
antithrombotic therapy after successful ablation.Warfarin is required
for all AF ablation patients for 2–3 months post-procedure: those
with a sufficiently low preoperative CHADS2 score, or equivalent,
can resume aspirin therapy at the time, but patients with a score
of
≥
2 should continue with warfarin even after successful ablation.
Patients should be considered for ablation based on symptoms and
not based on a wish to stop warfarin.
References available on
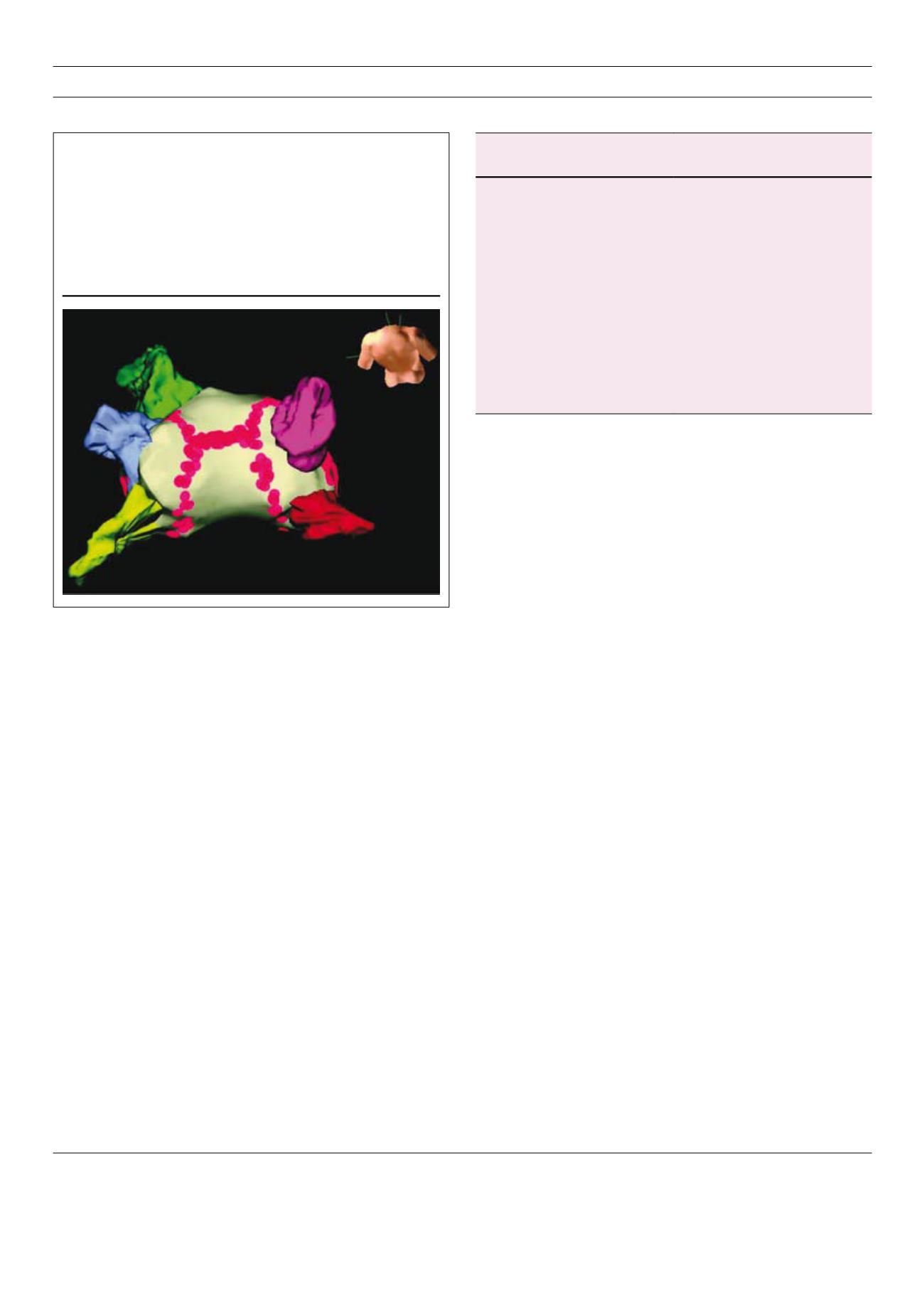
Figure 2:
3-D reconstruction of left atrium using NavX system (St
Jude Medical, MN, USA). The left atrium is seen from above
and behind, with left atrial appendage (green) top left.
Circumferential ablation (red dots) has been performed around
each pair of pulmonary veins (magenta, red; yellow, blue),
resulting in their electrical disconnection from the left atrium,
and a line of ablation created on the roof of the left atrium. This
map can be navigated in real time allowing reduced use of X-ray
fluoroscopy and accurate delivery of treatment.
NICE recommendations on initial strategy for treating AF
Rate control
Rhythm control
• minimal or no symptoms
• symptomatic
• persistent AF
• paroxysmal or persistent < 1 year
• > 65 years old
• younger patients
• coronary artery disease
• first presentation with lone AF
• contraindications to
anti-arrhythmic drugs
• AF secondary to a treated/
corrected precipitant
• unsuitable for cardioversion
• congestive heart failure*
• no congestive heart failure*
*based on subgroup data from AFFIRM and RACE – not supported (for drug-
based rhythm control) by AF-CHF data