VOLUME 8 NUMBER 1 • MARCH 2011
33
SA JOURNAL OF DIABETES & VASCULAR DISEASE
CUTTING EDGE OF DIABETES TECHNOLOGY
lin, which would mitigate against the inevi-
table insulin stacking that occurs
• a need for a robust interstitial blood glucose
sensor
• a need for a dual hormone pump where
glucagon is released and insulin delivery
suspended to prevent or treat hypoglycae-
mia
• algorithms that are fail safe and capable of
handling ALL real-world situations.
Patch pumps filled an entire session, with
the enticement of a much smaller, hopefully
cheaper insulin pump that can be worn on any
area of the body. The technology and behind-
the-scenes regulatory, legal and engineering
genius of these developments are mind blow-
ing. It is easy to envisage the benefits that
safe, simple delivery devices could offer to
thousands of people with diabetes. We await
the introduction of these new technologies as
eagerly as we await the inclusion of artificial-
intelligence algorithms that would make the
attainment of euglycaemia safer and easier.
However, hypoglycaemia remains a clear
and present danger to the attainment of per-
fect glycaemic control. Fear of hypoglycaemia
leads patients to run higher sugars and adopt
avoidance behaviours that sabotage long-term
control. Prof Phil Cryer (Mr Hypoglycaemia)
presented a paper at the session on hypogly-
caemia. It is now well recognised that hypogly-
caemia may account for between 4 and 10%
of the mortality in diabetes, with many of the
deaths being attributed to cardiac arrhythmias
rather that hypoglycaemic seizures and coma.
While an attempt was made to reach a consen-
sus of the exact value that defines hypoglycae-
mia, this has greater relevance for regulatory
authorities and clinical trials than it does for
real-world patient care. A value of 3.9 mmo/l
may be too high for clinical trials, but provides
a buffer zone for people with diabetes. It must
however be pointed out that there is not much
scientific support for this value.
Hypoglycaemia and its symptoms and con-
sequences vary from time to time in any given
patient and probably are best defined by a
range of blood sugars rather than an absolute
value. This range needs to be tailored to the
clinical situation, the age of the patient, the
duration of disease and concomitant medical
problems. Lessons learned from both inpa-
tient (NICE-SUGAR) and outpatient (ACCORD,
VADT) clinical trials targeting very strict glucose
control have resulted in unexpected increases
in morbidity and mortality.
A particular concern is the entity of hypo-
glycaemia-associated autonomic failure and
hypoglycaemia unawareness. In elegant PET
scan studies of humans with and without
hypoglycaemia unawareness, there appears to
be a loss in perception of any noxious stimulus
related to hypoglycaemia in those with hypo-
unawareness. The net effect is that these indi-
viduals do not feel their hypos but in particular
will take no evasive action to avoid such epi-
sodes, even if they are made aware of them,
because they do not feel bad with them. This
helps to explain the difficulties faced in trying
to ‘re-train’ these individuals to run higher
sugars and feel their lows, and the high rate of
refractory hypo-unawareness.
A particularly interesting session on multi-
modal treatment of type 2 diabetes covered
the use of leptin combined with amylin in
reducing glycaemic variability, possibly through
the regulation of gastric emptying and incre-
tin hormone induction. A brief but interesting
mention of the role of glucagon in mainte-
nance of dysglycaemia again raised the notion
that glucagon targeting may be a therapeutic
option.
However, the most interesting session was
on the possibility, or better yet the probabil-
ity of curing type 2 diabetes with surgery. The
benefits of gastric bypass procedures were
presented to look like a treatment panacea for
the myriad of disorders associated with obesity
and insulin resistance, or rather should we say
that stem from hyperinsulinaemia. The con-
cept of a ‘gastric diabetogenic factor’ (GDF)
was raised and supported. It certainly sounds
plausible that the contact of food with entero-
cytes in the gastric mucosa could lead to the
release of this GDF, which results in a state of
hyperinsulinaemia and with it all of the well-
described consequences of hyperinsulinaemia.
Watch this space...
Finally, tucked away in a single lecture,
seemingly out of place, was a talk on biosimi-
lar insulins. It was my impression that from an
organising committee standpoint, they could
no longer ignore the elephant in the room and
were forced to make some mention of them.
This, while remembering that conferences of
this type could not be held without the sig-
nificant financial support of those companies
driving the new developments and new drugs.
It was estimated that by the year 2018, bio-
similar insulin would have eroded the normal
insulin market by some six billion dollars. Bio-
similar insulins at a cost of $6.75 per 1 000 IU
versus $32.00 per 1 000 IU for normal insulin
would make them hard to ignore. The impres-
sion I got from the moderators was distinctly
negative towards biosimilar insulins.
I can only think back to the discovery of
insulin in 1922 when Banting was offered mil-
lions of dollars by a Wall Street consortium to
sell the rights to insulin. Sir Frederick Banting
at best was struggling financially but he held
firm, dismissing the offer, saying that ‘the indi-
gent diabetic is our greatest problem. Every
effort must be made to reduce the cost of
insulin and remove the necessity of expensive
diets so that they can look after themselves’. I
would venture to say that more lives are lost
today because insulin could not be accessed
than are lost to the devastating complications
of the disease. While it is scientifically laudable
to push the frontiers to develop new designer
drugs and gadgets to normalise blood sugars,
we should never forget the many lives that are
lost because patients never got a chance to
sample the ‘unspeakably wonderful’ benefits
of insulin.
David Segal
Paediatric endocrinologist, CDE, Parktown,
Johannesburg
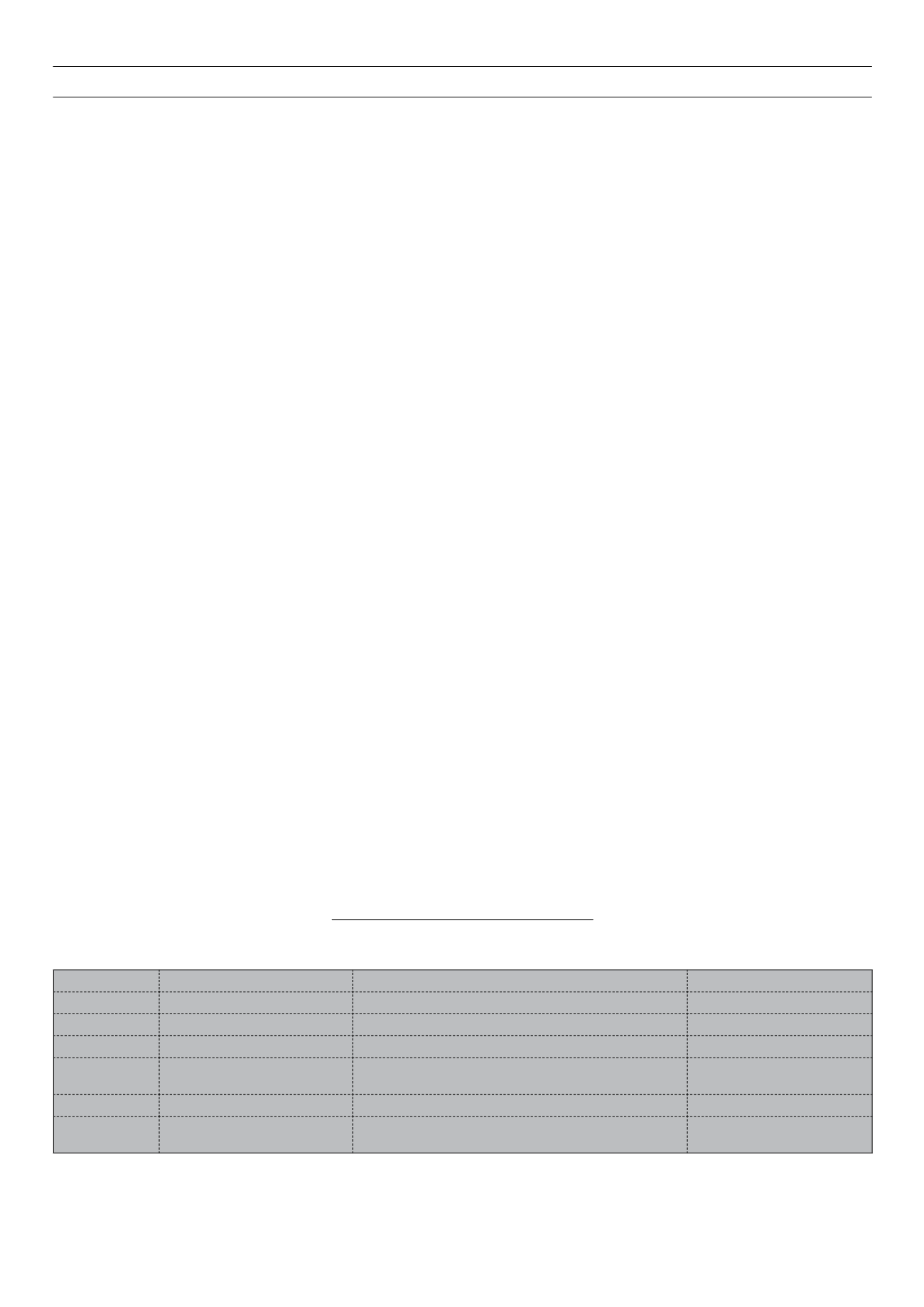
Diary for 2011 diabetes congresses
DATE
PLACE
CONFERENCE
WEBSITE
9–11 April
UFS, Bloemfontein
SEMDSA, LASSA, DESSA congress
24–28 June
San Diego, California, USA
71st American Diabetes Association (ADA)
22–24 July
Johannesburg, SA
13th CDE Postgraduate Forum in Diabetes Management (CDE)
1–2 September
Berlin, Germany
4th EPCCS annual scientific meeting for primary care in
cardiovascular disease
12–16 September Lisbon, Portugal
47th EASD meeting
4–8 December
Dubai International Convention &
Exhibition Centre Dubai, UAE
IDF World Diabetes congress