DRUG TRENDS
SA JOURNAL OF DIABETES & VASCULAR DISEASE
38
VOLUME 8 NUMBER 1 • MARCH 2011
Dr Kramer said.
The search for a common aetiology for the
metabolic syndrome was first grounded in
insulin resistance but this unifying aetiology
has remained unproven. Subsequently, visceral
obesity, inflammation and hyper-insulinaemia
were explored as a common aetiology, but
these attempts also failed. So there was no
real advantage in calling these conditions the
metabolic syndrome’, Dr Kramer explained.
At the practical level of general practitioner
and patient communication, the cluster of dys-
glycaemia, hypertension and dyslipidaemia in
the presence of visceral obesity may perhaps
usefully be described as ‘the syndrome that
was once known as the metabolic syndrome’,
Dr Larry Distiller added.
The changing gut microbiome: is it
killing us?
In a journey to look at childhood obesity differ-
ently and in the context of the increase in both
type 1 and type 2 diabetes, Dr David Segal,
paediatric endocrinologist with academic com-
mitments at Wits University Medical Faculty
and also in private practice at CDE, Parktown,
explored the available medical literature and
interpreted new data to provide concepts for
clinical intervention.
He targeted two main features of modern
obesity: firstly, neuro-economics (the cost–ben-
efit of obtaining food), and secondly, the con-
sequences of increased fat and carbohydrate
intake, which are challenging the
β
-cell and
altering the gut microbiota so that food transi-
tion and absorption is modified. ‘While genetic
studies have added to our knowledge of the
gene control of appetite, satiety and feedback
mechanisms, they have failed to give us a prac-
tical option to control obesity’, he said.
The field of neuro-economics applied
to food calculates the price-cost in energy
expended, and the risk and effort to procure
the food that we eat, and relates it to demand,
which is ever present as appetite, and supply,
which in urban areas is plentiful at the nearest
supermarket.
‘In neuro-economic terms, our food is very
cheap and is extra-ordinarily palatable, thereby
stimulating excess demand. This demand
will remain consistently high unless we can
increase the energy-risk cost or reduce the pal-
atability’.
1
‘In effect, this means that we cannot
control obesity in our modern urban setting’,
Dr Segal pointed out.
In a study on the burden of diabetes among
American youth, the SEARCH study
2
has
shown the rising prevalence of type 2 diabe-
tes in different racial groups in six states in the
USA. Among younger children from birth to
nine years of age, type 1 diabetes accounted
for approximately 80% of diabetes cases,
while among the older group (10–19 years)
type 2 diabetes ranged from 6% in the non-
Hispanic whites, to 76% (1.74% per 1 000
cases) among American Indians.
Interestingly, the only group in the 15- to
19-year-olds to show the same prevalence
(3/1 000) for both type 1 and type 2 diabetes
was the African-American female population.
‘Type 2 diabetes in adolescents is associated
with increased obesity, with a five-year lead
time between obesity
occurrence (BMI
≥
30
kg/m
2
) and the devel-
opment of diabetes’,
Dr Segal noted.
In evaluation of
the rising trend of
childhood type 1
diabetes, there is an
association with rising
childhood
obesity.
Up until the 1950s,
diabetes was seen
as a single disorder
with an aggressive
presentation in the
young. ‘In the 1960s,
scientific
evidence
saw the emergence
of an auto-immune
basis for type 1 dia-
betes with lympho-
cytic infiltration of the
islets, a human leukocyte antigen (HLA) link to
diabetes and islet antibodies. We do not have
a clue as to what triggers the immune system
to attack the
b
-cell’, Dr Segal said.
An hypothesis that is gaining credence is
the ‘accelerator’ hypothesis which proposes
that weight and associated insulin resistance
accelerate loss of
b
-cells in both type 1 and
type 2 diabetes and the only thing that distin-
guishes these two forms of diabetes is the rate
of progression. There is considerable evidence
that weight gain in early life can be used to
predict at two years of age the risk of islet
immunity in children with first-degree relatives
with type 1 diabetes.
3
Also, over the past 20
years, there has been a steady increase in BMIs
in girls and boys at the time of diagnosis of
their type 1 diabetes.
4
‘If we look at HLA risk markers for diabetes,
it is evident that there are genotypes that are
related to the development of type 1 diabetes,
1.5 latent autoimmune diabetes in adulthood
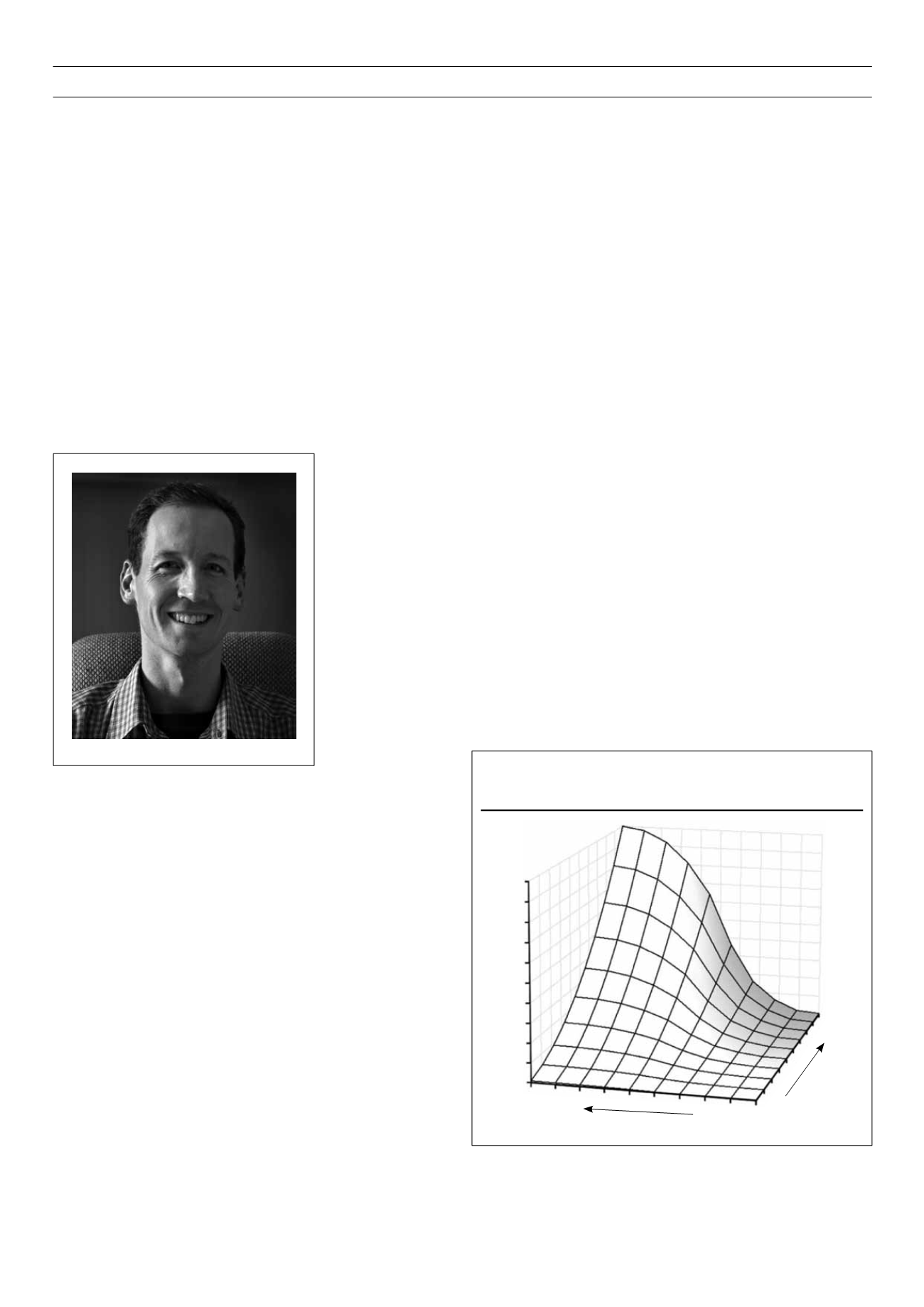
(LADA) and type 2 diabetes’, Dr Segal said.
Because of environmental pressures, a lower
predisposing genetic component is needed
today to result in the development of diabe-
tes than was required in the 1930s. ‘The pre-
disposing reactive genotype leads in fact to a
faster tempo of
b
-cell loss in the presence of
increasing insulin resistance’, Dr Segal pointed
out (Fig. 1).
In adolescents, it is the ongoing weight gain
that predicts the development of type 2 diabe-
tes rather than glucose levels, insulin resistance
Dr David Segal
Figure 1.
Relationship between the accelerator genotype, insulin resistance
and the probability of diabetes.
Probability of diabetes
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
Insulin resistance
Accelerator genotype