SA JOURNAL OF DIABETES & VASCULAR DISEASE
RESEARCH ARTICLE
VOLUME 14 NUMBER 2 • DECEMBER 2017
55
Cameroon
30
and Tanzani,
31
although lower than in ours.
The higher prevalence of overweight, obesity (abdominal and
general) as reflected in WC and mean BMI, hypercholesterolaemia,
alcohol abuse and smoking, being more common in diabetic than
non-diabetic subjects, is however an expected finding, as they
all have individual and associative effects in predisposition to the
development of diabetes.
8,30
Therefore, while diabetes in itself
has been demonstrated to be an independent cardiovascular risk
factor,
32
the impact of its association or cumulative effect with other
traditional risk factors in the development, progression, morbidity
and mortality linked with CVDs cannot be overemphasised.
Limitations and strengths of the study
Our study has several limitations that deserve mention. First the
hospital base of the recruitments and the selected nature of the
participants could have increased the chances that those included
were at high risk for metabolic risk factors, which therefore could
account for the high prevalence of cardiometabolic risk factors
in our study. Secondly, the method of diagnosis of hypertension
could be subject to debate, but it has been clearly evidenced by
Burgess
et al
. that failure to carry out multiple measurements to
confirm the diagnosis may lead to false positives.
33
Thirdly, quantity
or concentration of alcohol in the local beer may vary from
one country to another, and we could not assess non-industrial
alcoholic beverages. Lastly, although the overall sample size was
large, the number of patients contributed from each participating
centre within the countries tended to be small, therefore precluding
meaningful centre-level analysis.
In spite of these limitations, the multi-centre, multi-national
character of this study increased our chances of adequately exploring
the prevalence of cardiometabolic risk factors in the participating
countries, anddemonstratingevidenceof thegrowingcardiovascular
risk factors in this region plagued with communicable diseases. The
use of well-trained data collectors (medical practitioners) also gave
confidence in the measured parameters.
Conclusions
This study reports alarmingly high prevalences of cardiometabolic risk
factors among adults presenting at urban and semi-urban hospitals
in selected countries in SSA, which is in line with IDF projections
of NCDs (hypertension and diabetes mellitus) in the region. It
also raises the question of the influence of rapid urbanisation on
the development of risk factors for imminent cardiovascular and
metabolic diseases. This has considerable public health impact
for an already economically disadvantaged setting to design new
methods or further strengthen existing measures and interventions
for the control of chronic diseases in the region.
We thank all the investigators who participated in data acquisition:
from Madagascar: Rakotoarisoa Bodosoa, Raharimanana Lanto,
RakotoarimananaJeanJacques,RatavilahyRoland,Andrianandrasana
Hery, Rabarijoelina Claude, Rakotoarisoa Holiarivelo, Johanes Abel,
Rakotoniaina Beatrice, Razafindramiandra Jacky, Raheliarisoa
Julia, Rabetrano Alice, Rasolonjatovo Methouchael, Miandrisoa
Rija Mikhael, Rakotozafy Joseline, Raveloarison Marguerite,
Ramiandrisoa Bodovololona, Randriamiarisoa Ny Aina, Raniriharisoa
Voahirana, Rasolofomanana Ndrina, Rasamimanana Nivo Nirina
and Randriantsoa Eric; from Cameroon: Nzundu Anne, Mfulu Papy,
MumbuluErick,ChristianNsimbaLuzolo,MrBoderalFundu,Tswakata
Masam, Iwnga Kabenba, Lepica Bonpeka, Murielle Longokolo,
Tondo, Bandubola Dedie, Kahamba Jean Louis, Massamba Mp Cla,
Loshisha-Armod, Bhuvem, Nzambi Mpvngv Stephane, Jimm Pierre
K and Toure Wenana Parfait; from the Democratic Republic of
Congo: Toko Olivier, Nzundu Annie, Tswakata Masam, Musibisoli
Dieudonne, Longokolo Mireille, Bandubola Dedie, Kahamba Jean-
Louis, Massamba Mpela and Loshisha Arnold.
We also thank the staff of the Clinical Research Education,
Networking and Consultancy (CRENC), Cameroon for their
assistance in data analysis and interpretation, and for drafting the
manuscript. We acknowledge funding support from Sanofi Aventis
pharmaceuticals.
References
1. Kengne AP, Mayosi BM. Readiness of the primary care system for non-
communicable diseases in sub-Saharan Africa.
The Lancet Global Health
2014;
2
(5): e247–248. PMID: 25103156.
2. Mensah GA. The global burden of hypertension: good news and bad news.
Cardiology Clinics
2002;
20
(2): 181–185. PMID: 12119794.
3. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global
burden of hypertension: analysis of worldwide data.
Lancet
2005;
365
(9455):
217–223. PMID: 15652604.
4. Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden
of undiagnosed hypertension in sub-Saharan Africa: a systematic review and
meta-analysis.
Hypertension
2015;
65
(2): 291–298. PMID: 25385758.
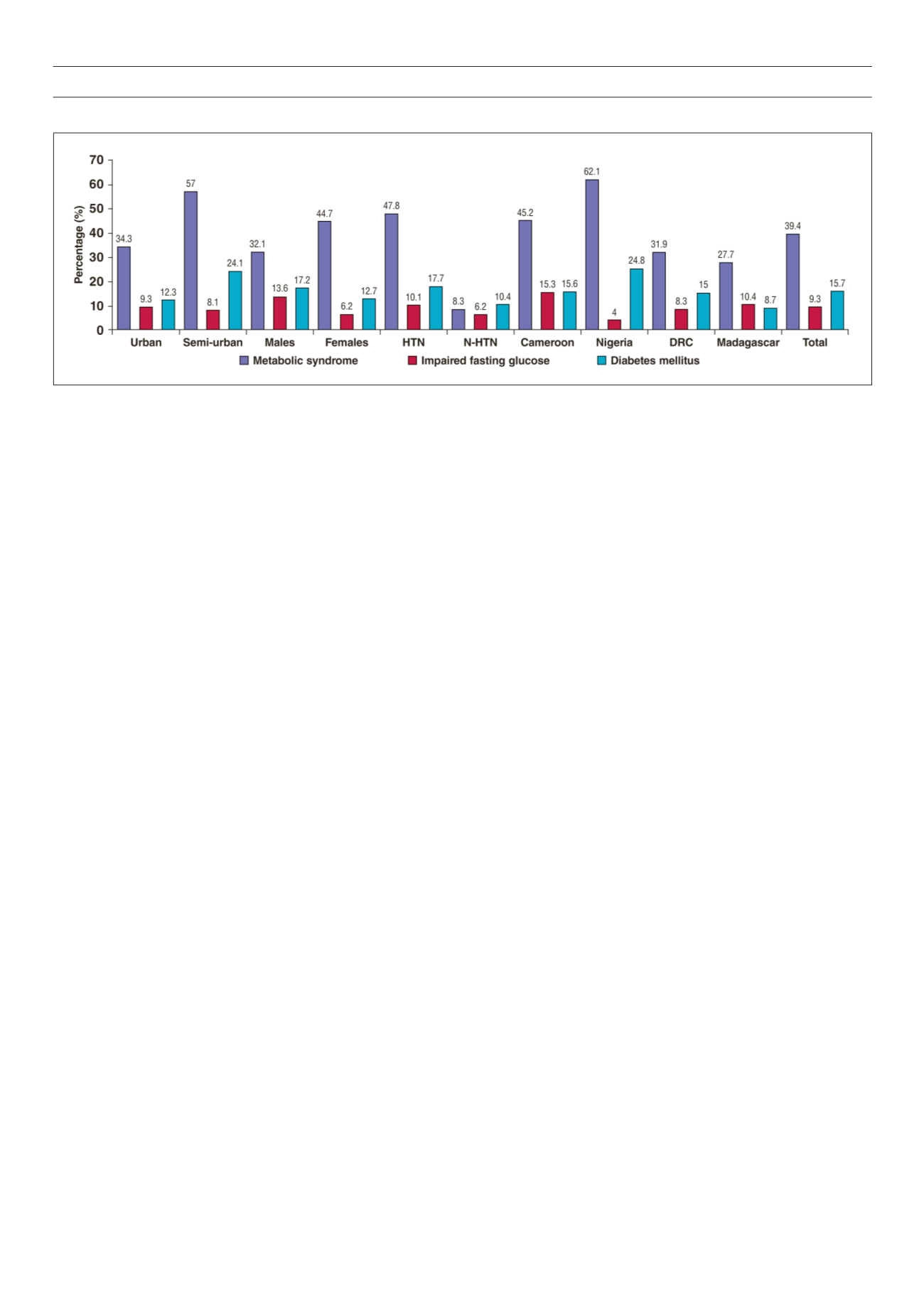
Figure 1.
Prevalence of the metabolic syndrome, impaired fasting glucose levels and diabetes across countries, urbanicity, gender and hypertension status. HTN =
hypertensives, N-HTN = non-hypertensives



















