RESEARCH ARTICLE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
54
VOLUME 15 NUMBER 2 • NOVEMBER 2018
baseline values. LDL level showed a 58.5% decrease at the end of
the 12 months compared to baseline value, whereas no change
was observed in HDL levels. While a statistically significant increase
was observed in the brachial artery basal diameter and hyperaemia
diameter compared to baseline values, no change was observed in
the post-nitrate diameter and EID values. FMD showed a statistically
significant increase compared to baseline (Table 2).
No statistically significant difference was found between
the atorvastatin and rosuvastatin groups in respect of baseline
transthoracic echocardiographic and brachial artery endothelial
function measurements (Table 3). Comparison between the two
groups in terms of their effects on non-invasive ultrasonographic
brachial artery measurements after one year revealed no statistically
significant difference. However, a significant difference was observed
in hyperaemia diameter in favour of rosuvastatin (Table 4).
Percentage changes in non-invasive brachial arterymeasurements
after 12 months of treatment were compared between the two
groups. A statistically significant difference was found in percentage
change in the rosuvastatin group’s brachial artery post-nitrate
diameter (
p
< 0.05). Non-significant changes were found in the
basal diameter and hyperaemia velocity in favour of the rosuvastatin
group (
p
= 0.089 and
p
= 0.088, respectively) (Table 5).
Discussion
This study revealed that both atorvastatin and rosuvastatin had an
effect on baseline lipid values, brachial artery basal diameter and
hyperaemia diameter, and FMD and EID measurements. Comparing
12-month non-invasive measurements of atorvastatin and
rosuvastatin groups, it was found that the statins had similar effects
on endothelial function in the subjects with hyperlipidaemia.
Post-nitrate diameter in the rosuvastatin group was significantly
improved at the end of the 12-month treatment compared to
baseline values. Endothelial dysfunction is one of the early functional
markers of atherosclerosis.
11,12
Preventative measurements should
be taken before clinical manifestation of atherosclerotic events. For
this reason, detection of early atherosclerotic changes is of great
importance in reducing risk factors. Endothelial dysfunction can be
detected via FMD, a non-invasive, easily applicable and repeatable
method. Studies have demonstrated that FMD was correlated
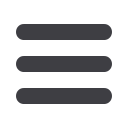
Table 2.
Post-treatment versus baseline values in the rosuvastatin group
Rosuvastatin
Baseline
12 months
p
-value*
Basal diameter (mm)
4.0 ± 0.5
4.2 ± 0.5
0.003
Hyperaemia diameter (mm)
4.4 ± 0.5
4.6 ± 0.5
< 0.001
NTG diameter (mm)
4.6 ± 0.5
4.7 ± 0.5
0.687
FMD (%)
9.7 ± 3.4
12.7 ± 3.7
< 0.001
EID (%)
16.8 ± 5.8
18.2 ± 5.8
0.105
TC (mg/dl)
271.2 ± 35.7 188.4 ± 44.8 < 0.001
(mmol/l)
(7.02 ± 0.92)
(4.88 ± 1.16)
TG (mg/dl)
173.5 ± 55.2 143 ± 54.1 < 0.001
(mmol/l)
(1.96 ± 0.62)
(1.62 ± 0.61)
LDL-C (mg/dl)
180.5 ± 26.1 105 ± 39.2 < 0.001
(mmol/l)
(4.67 ± 0.68)
(2.72 ± 1.02)
HDL-C (mg/dl)
56.8 ± 13.6
54 ± 11.5
0.093
(mmol/l)
(1.47 ± 0.35)
(1.40 ± 0.30)
AST (U/l)
22.8 ± 6.7
23.3 ± 6.5
0.819
ALT (U/l)
22.8 ± 9.7
23.6 ± 9.3
0.759
CPK (U/l)
94 ± 31.3
116 ± 73.8
0.007
*Student’s
t
-test,
p
< 0.05.
SD: standard deviation; NTG: post-nitrate; FMD: flow-mediated dilation; EID:
endothelium-independent dilation; AST: aspartate transaminase; ALT: alanine
transaminase; CPK: creatinine phosphokinase; TG: triglycerides; TC: total
cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density
lipoprotein cholesterol.
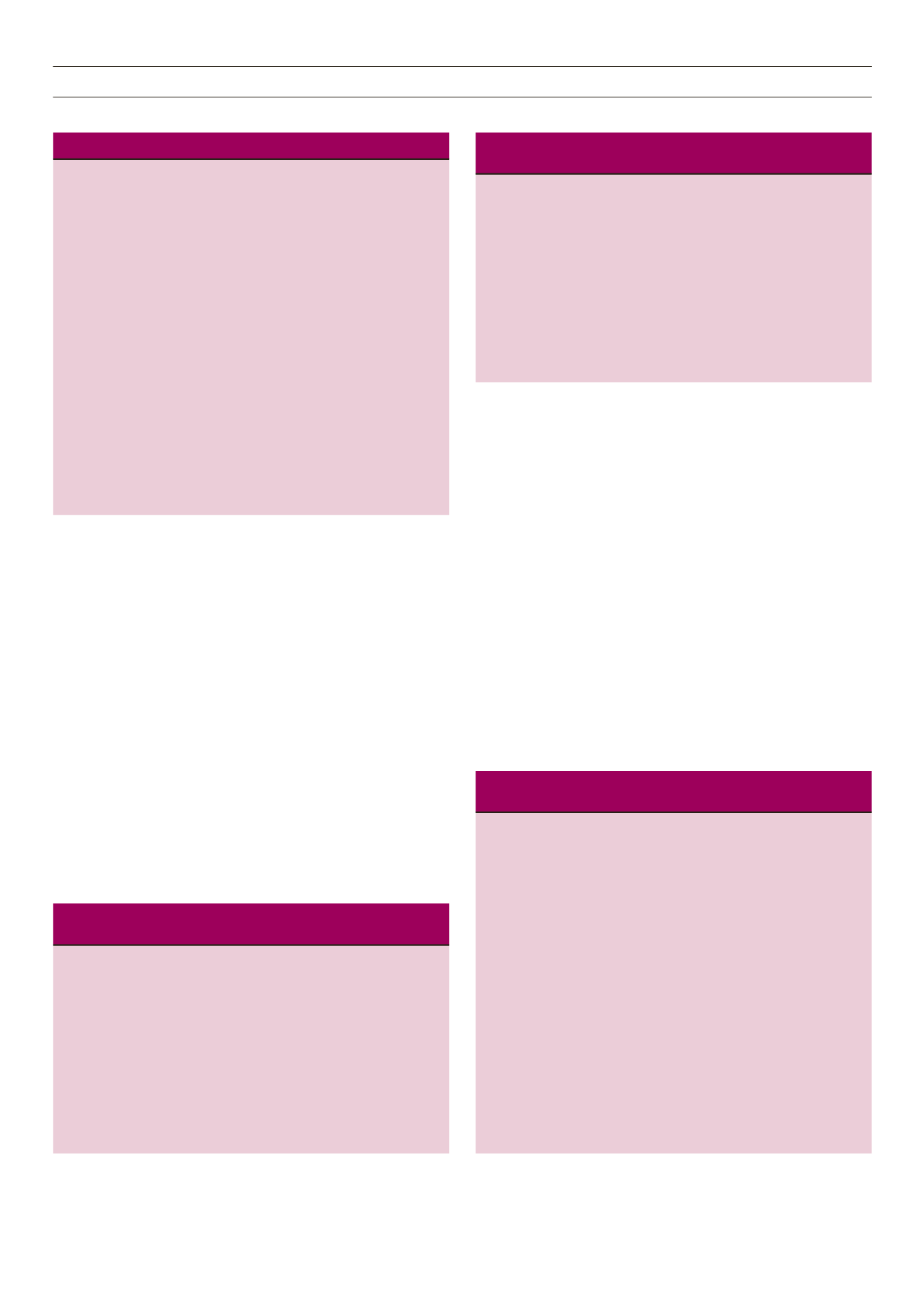
Table 4.
Rosuvastatin versus atorvastatin in terms of non-invasive test
results after 12 months of statin therapy
Brachial artery
Atorvastatin Rosuvastatin
measurements after therapy group (
n
= 50) group (
n
= 54)
p
-value*
BA basal diameter (mm)
4.01 ± 0.6
4.02 ± 0.5
0.850
BA basal velocity (cm/s )
71.95 ± 14.8
79.32 ± 16.9
0.240
BA hyperaemia diameter (mm)
4.34 ± 0.6
4.43 ± 0.5
0.404
BA hyperaemia velocity (cm/s)
72.21 ± 15.9
73.4 ± 16.3
0.713
BA NTG diameter (mm)
4.6 ± 0.6
4.69 ± 0.5
0.451
BA NTG velocity (cm/s)
68.92 ± 15.4
68.23 ± 15.5
0.833
BA FMD (%)
8.52 ± 3.3
9.71 ± 3.4
0.750
BA EID (%)
15.31 ± 5.1
16.84 ± 5.8
0.159
*Student’s
t
-test,
p
< 0.05.
SD: standard deviation; BA: brachial artery; NTG: post-nitrate; FMD:
flowmediated dilation; EID: endothelium-independent dilation.
Table 5.
Changes in brachial artery measurements after 12 months of
treatment in the atorvastatin versus rosuvastatin group
Change in
brachial artery Atorvastatin group Rosuvastatin group
measurements
(
n
= 50)
(
n
= 54)
after therapy Median (25–75%)
Median (25–75%)
p
-value*
BA basal
0.011 (–0.041–0.031) 0.010 (–0.007–0.045) 0.089
diameter (mm)
BA basal
0.001 (–0.119–0.157) –0.043 (–0.206–0.378) 0.120
velocity (cm/s)
BA hyperaemia
0.018 (–0.034–0.060) 0.021 (0.011–0.048) 0.644
diameter (mm)
BA hyperaemia 0.056 (–0.087–0.0347) –0.012 (–0.168–0.116) 0.088
velocity (cm/s)
BA NTG
0.028 (0.008–0.045) 0.020 (–0.028–0.036) 0.045
diameter (mm)
BA NTG
–0.004 (–0.167–0.113) –0.020 (0.0113–0.088) 0.982
velocity (cm/s)
BA FMD (%)
0.203 (0.008–0.441) 0.193 (0.049–0.0433) 0.958
BA EID (%)
0.110 (–0.115–0.225) 0.037 (–0.460–0.347) 0.827
*Mann–Whitney
U
-test,
p
< 0.05.
BA: brachial artery; NTG: post-nitrate; FMD: flow-mediated dilation; EID:
endothelium-independent dilation.
Table 3.
Statistical comparison between atorvastatin and rosuvastatin
groups in terms of baseline brachial artery measurements
Baseline brachial artery
Atorvastatin Rosuvastatin
measurements
group
group
p
-value*
BA basal diameter (mm)
4.01 ± 0.6
4.02 ± 0.5
0.850
BA basal velocity (cm/s )
71.95 ± 14.8
79.32 ± 16.9
0.240
BA hyperaemia diameter (mm)
4.34 ± 0.6
4.43 ± 0.5
0.404
BA hyperaemia velocity (cm/s) 72.21 ± 15.9
73.4 ± 16.3
0.713
BA NTG diameter (mm)
4.6 ± 0.6
4.69 ± 0.5
0.451
BA NTG velocity (cm/s)
68.92 ± 15.4
68.23 ± 15.5
0.833
BA FMD (%)
8.52 ± 3.3
9.71 ± 3.4
0.750
BA EID (%)
15.31 ± 5.1
16.84 ± 5.8
0.159
*Student’s
t
-test,
p
< 0.05.
SD: standard deviation; BA: brachial artery; NTG: post-nitrate; FMD:
flowmediated dilation; EID: endothelium-independent dilation.



















