VOLUME 15 NUMBER 2 • NOVEMBER 2018
69
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
SGLT-2 inhibitors in type 2 diabetes
Protecting the kidney (and heart) beyond glucose control
Brian Rayner
Correspondence to: Brian Rayner
Division of Nephrology and Hypertension University of Cape Town
e-mail:
brian.rayner@uct.ac.zaPreviously published by
deNovo Medica,
September 2018
S Afr J Diabetes Vasc Dis
2018;
15
: 69–73
Background
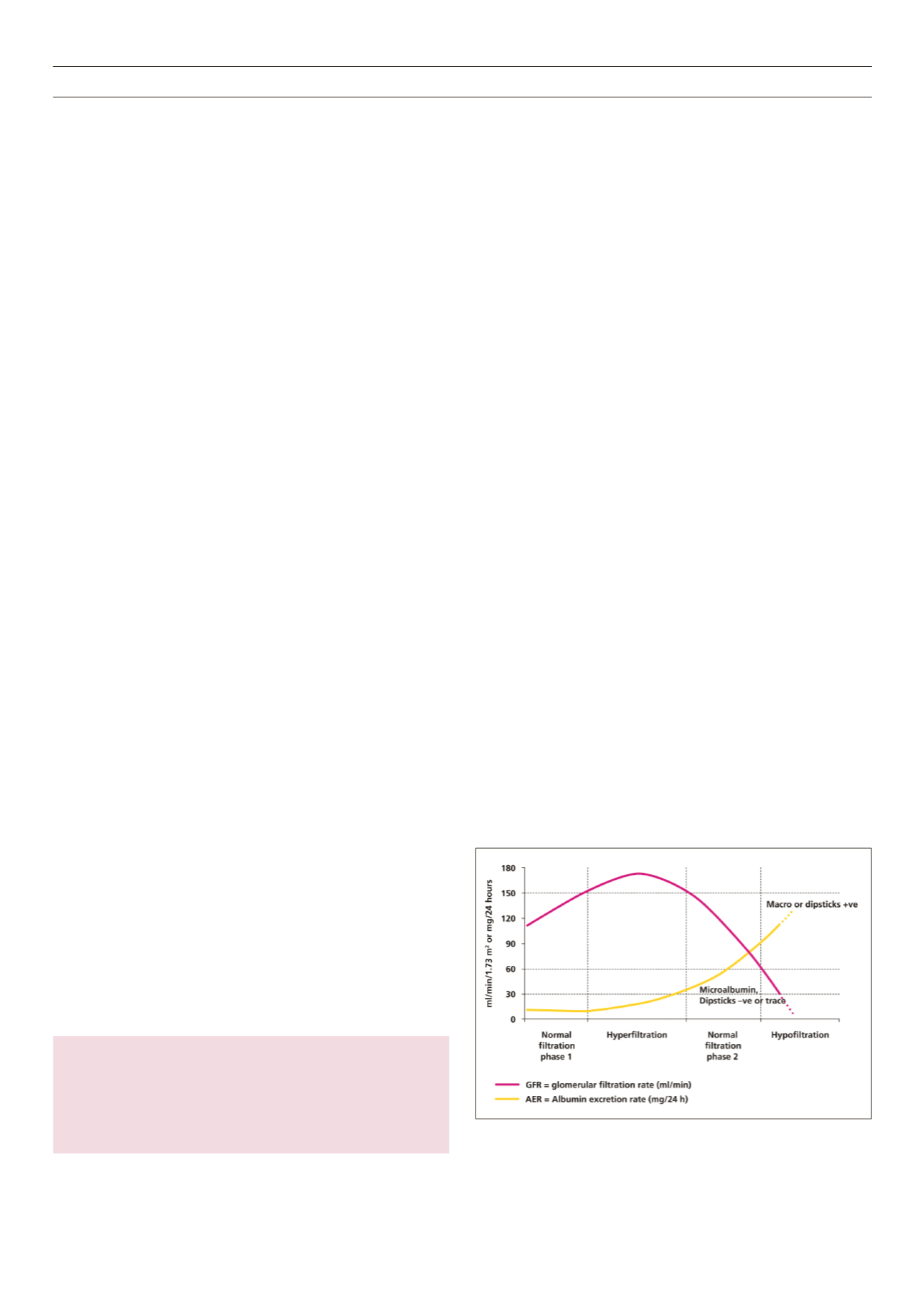
Longstanding diabetes is associated with both macrovascular
(myocardial infarction, stroke and peripheral vascular disease) and
microvascular disease (retinopathy, nephropathy and neuropathy).
Nephropathy affects approximately 40% of patients with diabetes
and follows a long natural history (Fig. 1), initially manifesting with
an elevated glomerular filtration rate (GFR) due to poor glucose
control.
1
In time there is a progressive and inexorable decline in
renal function to end-stage renal disease. However, because many
diabetics remain undiagnosed for many years, chronic kidney
disease (CKD) may be present at diagnosis.
Nephropathy is predicted by small amounts of albumin in
the urine (below dipsticks detection) or microalbuminuria that
progressively increases to overt albuminuria associated with loss
of kidney function. In the United Kingdom Prospective Diabetes
Study (UKPDS) the progression rate from normoalbuminuria to
microalbuminuria was 2% per year, to macroalbuminuria 2.8%,
and macroalbuminuria to elevated serum creatinine 2.3%.
2
The importance of diabetic kidney disease (DKD) is two-
fold. Firstly, it heralds a markedly increased mortality rate with
advancing kidney disease, mainly due to cardiovascular (CV)
disease. The annual death rate for normoalbuminuria is 0.7%,
microalbuminuria 2%, macroalbuminuria 3.5% and elevated
creatinine 12.1%.
2,3
If nephropathy develops at age 30 years,
life expectancy is reduced by 14.8 years in men and 16.9 years
in woman.
4
The reasons for the increased CV risk are complex
and involve both traditional risk factors, especially worsening of
hypertension, and non-traditional risk factors such as vascular
calcification, which is beyond the scope of this article.
Secondly, DKD is now the commonest cause of end-stage CKD
in most countries in the world and South Africa is no exception.
5
Currently 47.2% of dialysis patients in the private sector are
diabetics and the vast majority type 2. In the state sector the
figure is 11.2% and the implication of this is that the majority
of diabetics in the public sector are sent home to die of end-
stage CKD. The cost of dialysis in the private sector is in excess of
R200 000 per annum per patient and accounts for one of the
single biggest expenditures by medical aids in South Africa.
It is abundantly clear that CV disease and DKD are inextricably
linked, and both need to be addressed to reduce the burden of
kidney and associated CV disease.
Current knowledge of prevention and treatment
of DKD
There are many challenges in the treatment of DKD. Firstly, it is
silent and insidious with signs and symptoms only developing in
CKD stages 4 and 5; so late diagnosis is common. There is lack
of public awareness and failure to implement regular screening.
The major modifiable risk factors for DKD are the presence of
microalbuminuria (or incipient nephropathy), hypertension,
smoking, obesity, dyslipidaemia and dietary factors.
It is also critical to understand that small improvements in the
trajectory of GFR can translate into long-term benefits. For example,
by changing the trajectory of loss of GFR from 3 ml/min/year to 2
ml/min/year, the time to end-stage CKD can be increased by up to
10 years or more.
6
All diabetics should have their creatinine, estimated GFR (eGFR),
urine dipsticks, and urine albumin/creatinine ratio performed at
diagnosis andannually. If abnormal, theseneed tobeperformedmore
regularly. Dipsticks positive for albumin, macroalbuminuria, and/or
eGFR < 60 ml/min are very suggestive of DKD. Microalbuminuria
signifies incipient nephropathy and a very elevated eGFR > 120 ml/
min is also a risk factor because of the long-term harmful effects
of hyperfiltration.
Correct performance and interpretation of urinary albumin/
creatinine ratio are essential. Firstly, the urine should be a first
voided overnight specimen to standardise testing. Spot urines
significantly overestimate the presence of albuminuria. Ideally
three specimens need to be obtained, but in practice testing is
usually performed using only one. Normoalbuminuria is an albumin
creatinine ratio < 3 mg/mmol, microalbuminuria 3–30 mg/mmol
and macroalbuminuria > 30 mg/mmol (Table 1). Unfortunately
several laboratories report in gm of albumin to gm of creatinine,
Fig. 1.
Change in kidney function (GFR and albumin excretion) as diabetic
nephropathy progresses.



















