VOLUME 15 NUMBER 2 • NOVEMBER 2018
71
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
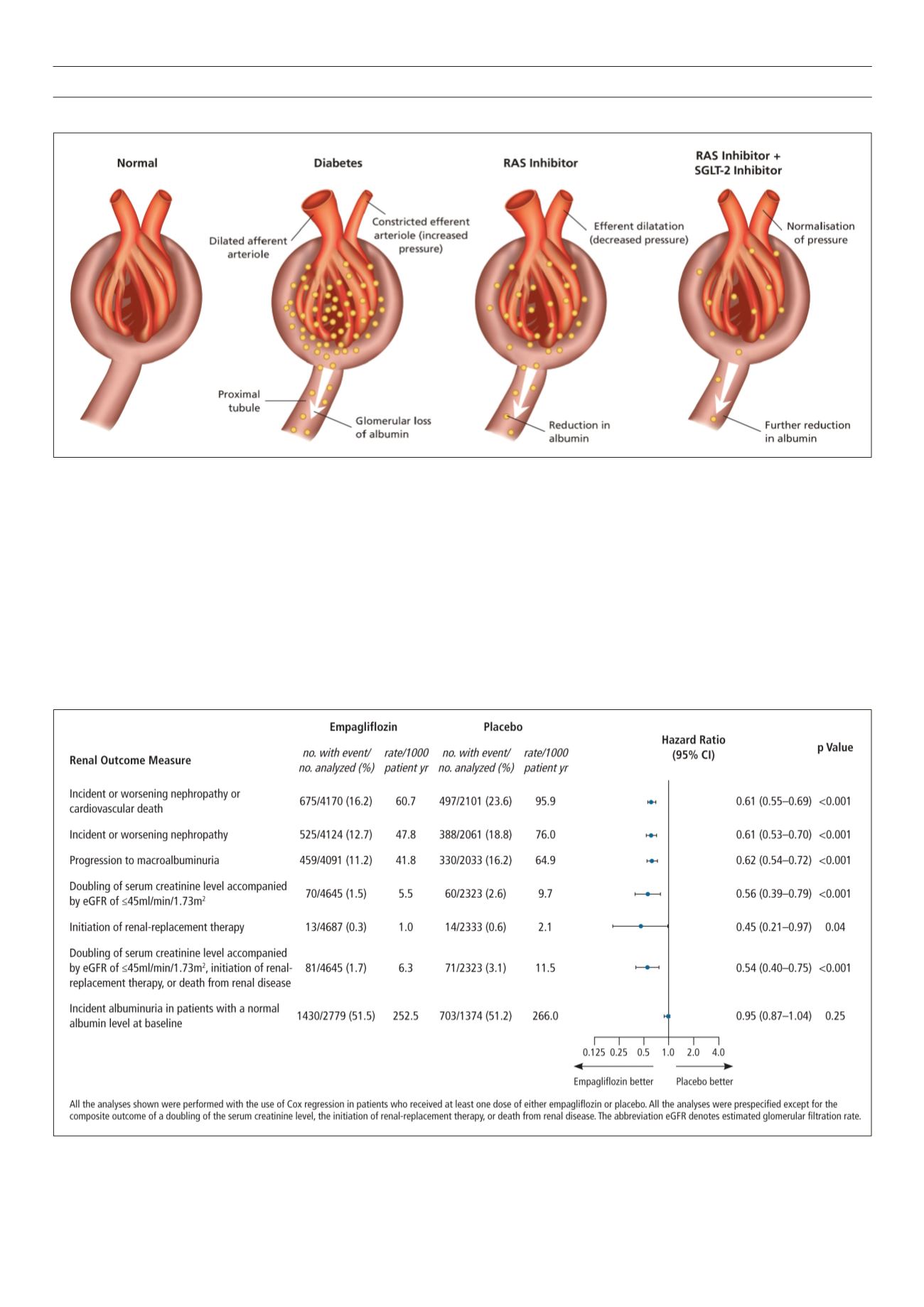
empagliflozin lowered HbA
1c
and body weight, and improved BP
control, but more importantly there was a 38% reduction in CV
death (
p
< 0.0001) and a 35% reduction in hospitalisation for HF
(
p
= 0.0017). From the kidney perspective, there was a 39%
reduction in new or worsening nephropathy (
p
< 0.001) and 46%
in hard renal end-points namely doubling in serum creatinine level,
initiation of renal-replacement therapy and death from end-stage
CKD) (
p
< 0.001).
21
The benefits were also seen in patients where the
estimated GFR was < 45 ml/min where there was a 44% reduction
in doubling of serum creatinine level (
p
= 0.0009) (Fig. 3).
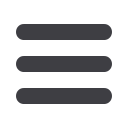
There was strong support that benefits accrued primarily due
to the underlying mechanism of action of empagliflozin and not
through glucose-lowering per se. Hospitalisation for HF separated
very early, suggesting that increased natriuresis was the primary
reason. Kidney benefit appeared after six months of treatment
and analysis of the eGFR showed early reduction in GFR in both
empagliflozin arms followed by a stable trend thereafter.
21
In
the placebo arm, there was no initial drop in eGFR, but this was
followed by an inexorable decline with the lines crossing at about
52 weeks. This supports the concept that reducing hyperfiltration
Fig. 2.
Nephron changes in diabetes and after administration of RAS inhibitor + SGLT2 inhibitor.
Fig. 3.
Risk compression for seven renal outcomes.
From EMPA-REG OUTCOME renal trial.



















