RESEARCH ARTICLE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
50
VOLUME 16 NUMBER 2 • NOVEMBER 2019
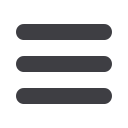
The results showed that 22% (
n
= 24) of the participants with
diabetes were at risk of falling (score < 19 of 24), compared to
only 1% (
n
= 1) in the control group. These findings show that
according to the DGI, one in five young to middle-aged adults with
diabetes were at risk of falling. The distribution of the DGI scores of
the cohort and control is illustrated in Fig. 1 and indicates that the
cohort group scored lower than the control group. The difference
in DGI score distribution between the groups was statistically
significant [t (166) = –6.14,
p
< 0.001].
The correlation between DGI scores (fall risk) and participants’
age demonstrated weak inverse correlations between DGI scores
and age (
r
= –0.29 and
r
= –0.37) for the cohort and control
groups, respectively. These correlation findings indicate that with
an increase in age there was a decrease in DGI score and therefore
a higher risk of falls.
Specific to the cohort group (paticipants with diabetes), the
correlation of the DGI scores with diabetes duration (years post
diagnosis) and control (glycaemic status) was also investigated and
findings showed a weak inverse correlation with diabetes duration
(
r
= –0.13) and diabetes control (
r
= –0.23). These findings indicate
that a longer diabetes duration in years and a higher glycaemic
status (uncontrolled diabetes) was correlated with a decrease in
DGI score and therefore a higher risk of falls.
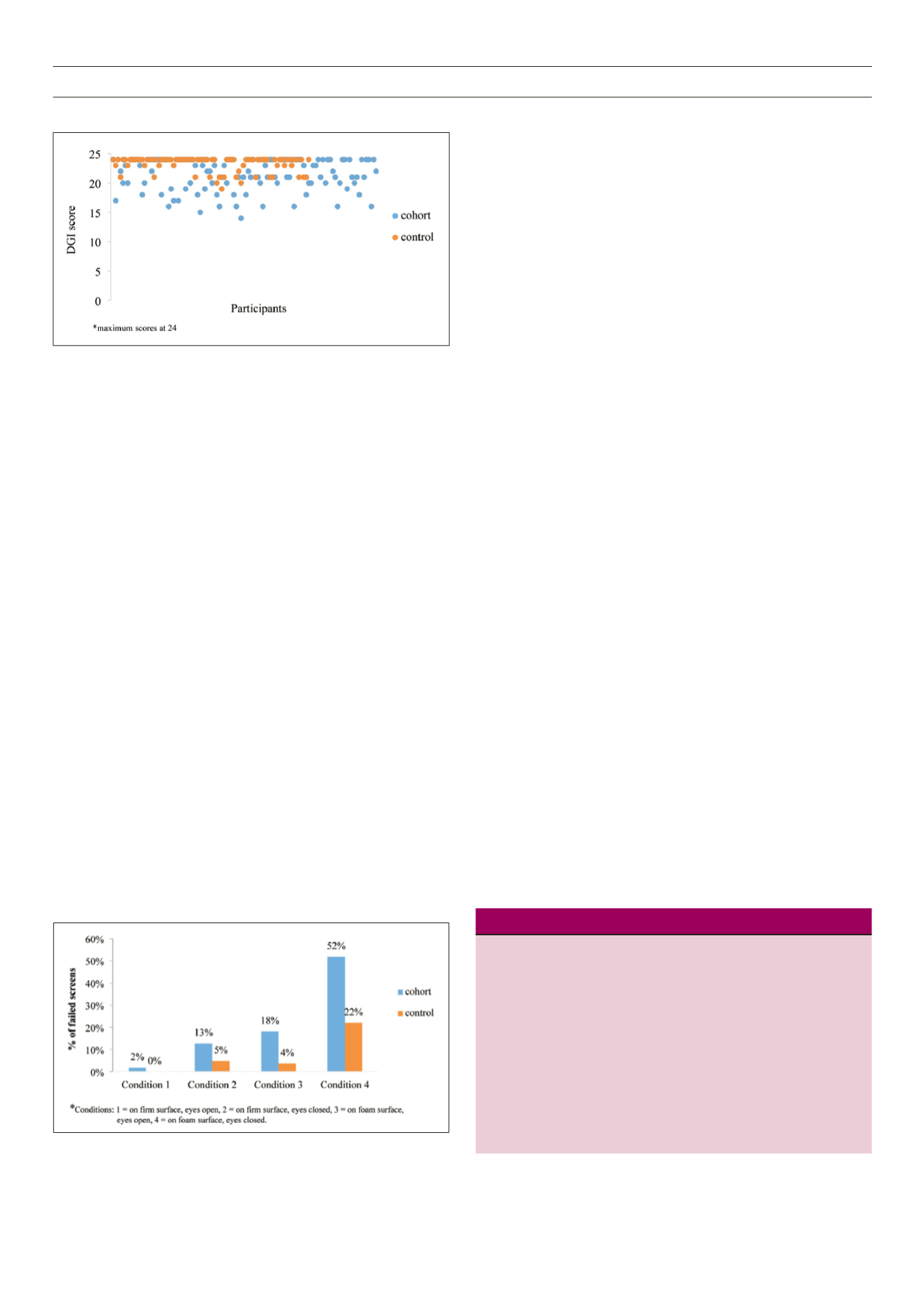
The M-CTSIB assessment was carried out under four conditions,
which were eyes open and closed, on foam and on a firm surface.
The use of foam disrupts proprioceptive cues, adding to the
challenge experienced by the vestibular system. Participants were
timed under each condition for their ability to maintain static
balance for the standard 30 seconds, and the total score was out
of 120 seconds.
14
Assessment findings showed 56 and 21% of the cohort and
control participants, respectively, failed to maintain static balance
for 30 seconds across all conditions and were at risk of falling.
M-CTSIB findings therefore showed that one in two young to
middle-aged adults with diabtes were at risk of falling, compared
to one in five in those without diabetes.
Participants at risk of falling in both groups mostly had
difficulties in condition three and four of the M-CTSIB screening,
where balance needs to be maintained with eyes closed and on the
foam, which demands more input from the vestibular system (Fig.
2). The difference in fall risk between the groups was statistically
significant [
t
(149) = –6.13,
p
< 0.001].
The correlation between M-CTSIB scores and participants’ age
indicated weak inverse correlations, with
r
= –0.29 and
r
= –0.14
for cohort and control groups, respectively. This indicated that
increasing age was related to a lower M-CTSIB score and a higher
fall risk. Specific to the cohort group, a weak negative correlation
with diabetes duration (
r
= –0.20) and diabetes control (
r
= –0.06)
was found, indicating that with longer diabetes duration (in years)
and a higher glycaemic status, a lower M-CTSIB score was obtained,
indicating a higher fall risk.
Participants with diabetes and possible complications presented
with a statistically significantly higher risk of falls compared to
those with diabetes and no complications (Table 1).
Discussion
This study aimed to determine fall risk in paticipants with diabetes
and compare that with a matched group of participants without
diabetes. Twenty-two per cent of the participants with diabetes in
this study were at risk of falling, based on their DGI scores. Similar
findings were reported in a previous study,
20
establishing that 38%
of their participants with diabetes, on symptom reports, experienced
instability when walking. The current study findings cannot ascribe
diabetes as the cause of the increased risk of falls, however other
authors explain that fall risk in patients with diabetes may be due
to pharmacological complications and peripheral neuropathy.
6,19
Our study also established that in participants with diabetes who
screened positive for diabetic peripheral neuropathy (
n
= 56), there
was more than a six-times higher fall risk, at 39%, compared to
those who screened negative (
n
= 54) at 6%.
The current study therefore established that young to middle-
aged South African adults (20–55 years) with diabetes were at risk
of falls. Furthermore, those with diabetes and co-morbidities were
at an even higher risk.
Table 1.
Diabetes complications and fall risk
Statistical
Statistical
difference
difference
Fall risk in DGI
Fall risk in M-CTSIB
Participants
with scores
with scores
with diabetes Number DGI
(
α
= 0.05) M-CTSIB (
α
= 0.05)
Positive for
neuropathy
56
22
0.3
40
0.9
Positive for visual
difficulties
62
15
50
Negative for
diabetic neuropathy 54
3
21
Negative for
visual difficulties
48
9
25
Fig. 1.
DGI score distribution.
Fig. 2.
M-CTSIB conditions.



















