RESEARCH ARTICLE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
54
VOLUME 16 NUMBER 2 • NOVEMBER 2019
Diabetic kidney disease (DKD) was defined as an estimated
glomerular filtration rate (eGFR) < 60 ml/min determined by
the CKD-epidemiology collaboration equation (CKD-EPI) and/
or a urine albumin/creatinine ratio (ACR) > 3 mg/mmol in the
absence of other causes of kidney disease. DR was defined as
the presence of aneurysms, bleeds, exudates and new vessel
formation on retinal examined by an ophthalmologist; DPN as the
presence of symptoms, loss of 128-Hz sensation and/ or abnormal
10-gm monofilament; and CVD as the presence of major adverse
cardiovascular events (MACE: coronary angioplasty, stent, coronary
artery bypass grafting, myocardial infarction or cerebrovascular
accident) and amputation (surgical removal of any part of a lower
limb due to diabetic causes).
SCH was defined as a thyroid stimulating hormone (TSH) level
> 4 mIU/l with a normal T4 and T3 level, and overt hypothyroidism
as a T4 less than the normal range (7.6–16.1 pmol/l) and TSH > 4
mIU/l. Thyroxine was given to all cases to maintain the T4 and TSH
level within the normal range. Diabetes was defined according to
the American Diabetes Association criteria.
7
Cases were excluded
if they were receiving amiodarone or lithium, or had had previous
thyroid surgery or ablation therapy.
The study was approved by the University of Cape Town,
Research Ethics Committee (331/2017).
Statistical analysis
Descriptive statistics were used to summarise total cohort
characteristics. For purposes of analysis, the cohort was divided
into black (Africans) and non-black (whites and other race groups).
Median with interquartile range was used to summarise continuous
variables, and frequency and percentages were used to summarise
categorical variables. Differences in continuous variables between
cases and control patients were compared using a Wilcoxon rank
sum test, while categorical variables were compared using Pearson
chi-squared test or Fisher’s exact test.
Logistic regression was used to determine associations,
magnitude and direction between the dichotomous T2DM
outcomes (DKD, CVD, DPN and retinopathy) and hypothyroidism,
adjusted for a priori selection of confounders and covariates. Highly
skewed continuous variables were log transformed prior to entering
into the model. Linear regression was used to assess associations
between eGFR and a priori selection of covariates. Goodness-of-fit
and influential observations were assessed after fitting each model.
All analyses were performed using Stata software (Version 14.2,
Stat Corp, College Station, TX).
Results
We identified 310 subjects, of whom 162 were controls and 148
were cases. All the hypothyroid cases were receiving thyroxine. The
overall demographics of the population are shown in Table 1. The
ethnic breakdown was predominantly white (84%), black (13%)
and other races (3%), and hypertension was present in 83% of the
hypothyroid group and 79% of the controls.
There were significant differences in the baseline characteristics
between the two groups. There were more females in the
hypothyroid group (60.8 vs 39.2%,
p
= 0.001) and fewer blacks
(10.8 vs 21.4%,
p
= 0.021) compared to controls. In addition the
mean age of the patients with hypothyroidism and duration of
diabetes was 65 vs 58 years (
p
< 0.001) and 13 vs 10 years (
p
=
0.001), respectively. T4 levels were slightly higher in the cases (12
vs 13.1 pmol/l,
p
= 0.004), but there was no difference in TSH level.
In respect of diabetic control, the cases had better glycated
haemoglobin (HbA
1c
) levels (6.9 vs 8%,
p
< 0.001) and used fewer
hypoglycaemic medications (
p
= 0.001) (Table 2). There were
differences in use of hypoglycaemic agents with more patients in
the control group receiving dipeptidyl peptidase-4 (DPP4) inhibitors
(40.1 vs 26.4%,
p
= 0.04), incretin mimetics (GLP agonists) (13 vs
6.1%,
p
= 0.01), and a trend towards more insulin use (51.9 vs
41.9.
p
= 0.08). There were no significant differences in the use of
metformin and sulphonylureas.
Regarding components of the metabolic syndrome, waist
circumference was not available, but in the cases, high-density
lipoprotein (HDL) cholesterol was significantly higher (1.1 vs
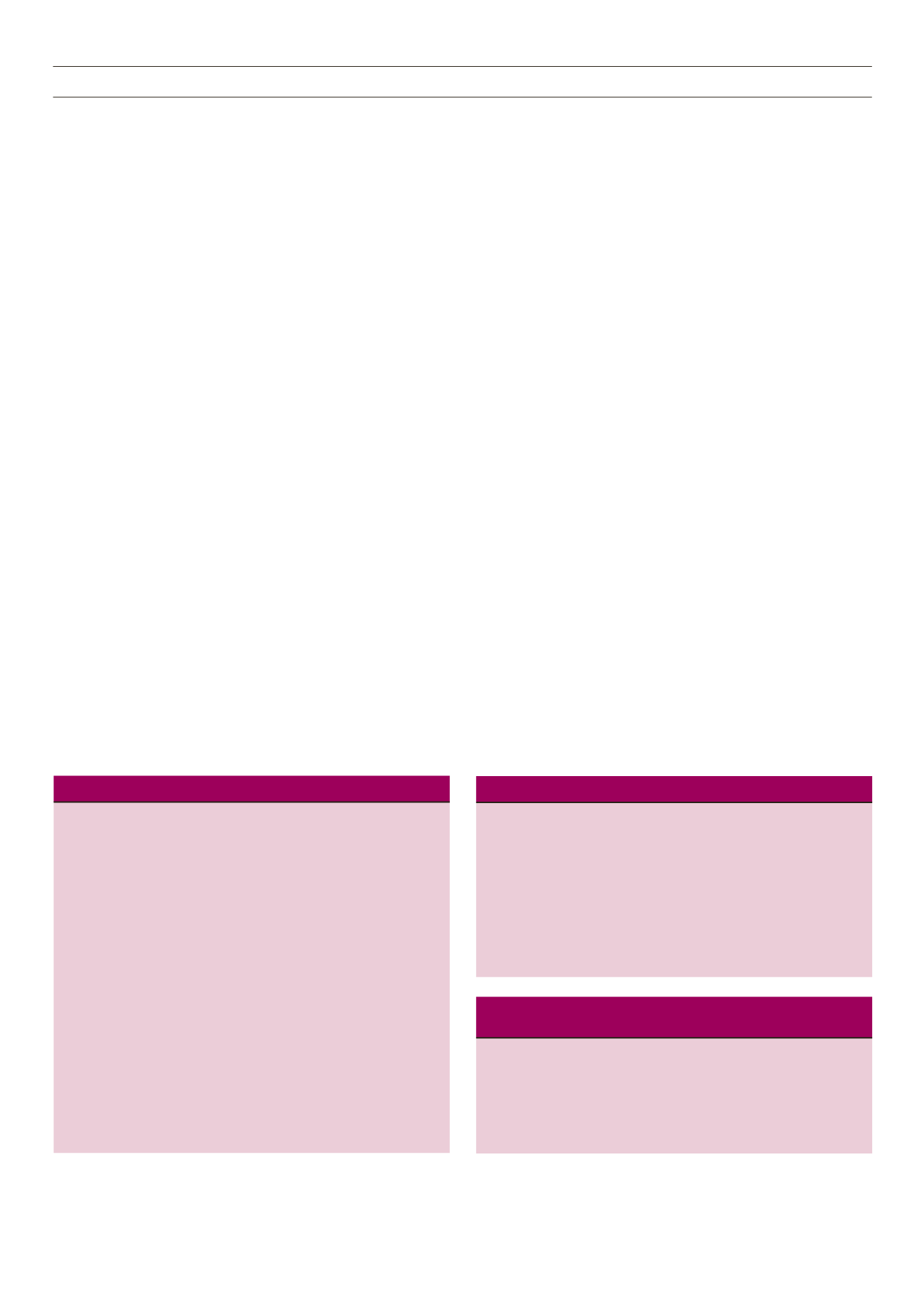
Table 1.
Demographics of the total group, cases and controls.
Total group Controls
Cases
Variable
(
n
= 310)
(
n
= 162)
(
n
= 148)
p
-value
Age (years)
62 (54–71)
58 (52–67)
65 (58–75) < 0.001
Gender,
146 (47.1)
98 (60.5)
48 (32.4)
< 0.001
male (%)
Race,
261 (84.2)
129 (79.6)
132 (89.2)
0.021
non-black (%)
Duration of
11 (7–18)
10 (5–16)
13 (9–19)
0.001
T2DM (years)
BMI (kg/m
2
)
34 (30–41)
34 (29–40)
34 (30–41)
0.370
HbA
1c
(%)
7.4 (6.3–9.1) 8.0 (6.7–9.6) 6.9 (6.1–8.7) < 0.001
TSH (mIU/ml)
1.6 (1.0–2.5) 1.6 (1.2–2.2) 1.6 (0.8–3.1)
0.973
T4 (pmol/l)
12.3 (11.–15) 12.0 (10–13) 13.1 (11–16.5) 0.004
Total cholesterol 4.5 (3.7–5.4) 4.5 (3.7–5.4) 4.4 (3.7–5.3)
0.776
(mmol/l)
Triglycerides
2.0 (1.3–2.8) 2.1 (1.4–3.2) 1.9 (1.3–2.6)
0.034
(mmol/l)
HDL-C (mmol/l)
1.0 (0.9–1.2)
1 (0.8–1.1)
1.1 (0.9–1.3)
0.001
LDL-C (mmol/l)
2.6 (2.0–3.2) 2.7 (1.9–3.3) 2.5 (2.0–3.2)
0.766
eGFR (ml/mim)
71 (55–88)
75 (58–90)
66 (52–82)
0.001
Urine ACR
1.8 (0.7–4.9) 1.6 (0.7–5.2) 2.0 (0.8–4.9)
0.717
(mgm/mmol)
Table 2.
Use of hypoglycaemic drugs in total group, cases and controls
No. of hypoglycaemic
drugs,
n
(%)
Overall
Controls
Cases
p
-value
1
101 (32.6)
38 (23.5)
63 (42.6)
0.001
2
122 (39.4)
66 (40.7)
56 (37.8)
3
67 (21.6)
46 (28.4)
21 (14.2)
4 20 (6.5) 12 (7.4) 8 (5.4)
Metformin,
n
(%)
254 (81.9)
135 (83.3) 119 (80.4)
0.503
Sulphonylurea,
n
(%)
93 (30.0)
52 (32.1)
41 (27.7)
0.399
GLP agonist,
n
(%) 30 (9.7) 21 (13.0) 9 (6.1) 0.041
DPP4 inhibitor,
n
(%)
104 (33.6)
65 (40.1)
39 (26.4)
0.01
Insulin,
n
(%)
146 (47.1)
84 (51.9)
62 (41.9)
0.08
Table 3.
Micro- and macrovascular outcomes between cases and con-
trols on univariate analysis
Total group Controls
Cases
Outcome (
n
, %)
n
= 310
n
= 162
n
= 148
p
-value
Amputation,
8 (2.6)
5 (3.1)
3 (2.0)
0.725
CKD (
n
= 297)
90 (30.3)
38 (24.7)
52 (36.4)
0.029
CVD
54 (17.4)
22 (13.6)
32 (21.6)
0.062
Neuropathy
148 (47.7)
79 (48.8)
69 (46.6)
0.706
Retinopathy (
n
= 75) 33/75 (44.0) 11/33 (33.3) 22/42 (52.4)
0.099



















