SA JOURNAL OF DIABETES & VASCULAR DISEASE
RESEARCH ARTICLE
VOLUME 16 NUMBER 1 • JULY 2019
15
of hospital workers in Nigeria have been reported to be physically
inactive.
23
However, a lower prevalence of physical inactivity has
been reported in earlier studies.
Of the 2 000 persons studied in Togo, 41%were sedentary, while
35% was reported from Bangladesh.
24,25
In a study among workers
at a medical college in Ghana, only 25% were physically inactive.
26
The reason for the disparity between our findings and those of
prior studies reporting low prevalence of physical inactivity may be
related to the highly selective nature of our study participants.
We noted the rarity of both active and passive cigarette smoking
in our participants. This is in keeping with previous reports that
document a paucity of smoking among Nigerians.
8,6,27
Generally,
this finding is in contrast to the findings in southern Africa, Asia
20,28
and the Western world,
29-31
where smoking constitutes a major
public health hazard.
Clustering of risk factors was prevalent in this study, with the
median number of risk factors being three (IQR 2–3) per participant.
This finding corroborates the findings of previous studies. In a study of
over 3 800 South African adults aged 50 years and above, Phaswana-
Mafuya and associates
32
reported a mean incidence of risk factors of
three. In a recent German survey, 45.1% of participants had multiple
risk factors.
33
Similar clustering has been reported by the SAGE wave
1 study that evaluated older adults across six countries.
34
A study among Senegalese private sector workers revealed that
more than half of the participants had two or more cardiovascular
risk factors.
35
Villegas and co-workers
36
reported that 67.6% of
men and women sampled across 17 general practice settings in
Ireland had more than one cardiovascular risk factor. This scenario
is the typical clustering in patients and deserves attention to reverse
or limit their contribution to NCD and its related mortality.
The prevalence of the selected NCDs parallels that obtained
in the literature from the Western world and the African region.
Hypertension was present in nearly half of the participants; CKD was
present in a little over a 10th of the population, and DM in nearly
a 10th. In the SAGE wave 1 study, the prevalence of hypertension
ranged from as low as 17.9% in Bangladesh to as high as 78% in
South Africa among older persons.
34
A prevalence of 47.2% was
reported among Irish hospital attendees in a study that evaluated
over 1 000 patients recruited from several general practices.
Oluyombo and colleagues,
37
working in south-west Nigeria,
reported a prevalence of 47.2% among residents of a semi-urban
community. A slightly lower prevalence of 31.4% was recently
reported from south-east Nigeria.
21
In a large community survey
that evaluated 5 206 adults in Malawi, Msyamboza and associates
38
reported a prevalence of 33% among persons aged 25 to 64 years.
A recent review by Bosu
7
demonstrated that the prevalence of
hypertension among workers in the West African sub-region has
steadily increased from 12.9% in the 1980s to 37.5% in 2014,
while figures up to 51.6% (95% CI: 49.8–53.4) and 43% (95%
CI: 42.1–43.9) have been recently reported in Nigeria among urban
and rural populations, respectively.
4
CKD, an emerging NCD, has gained attention in recent times as
it is both an end-point of communicable and non-communicable
diseases and a strong cardiovascular risk factor. It has become a
pandemic, affecting both developed and developing countries.
CKD was present in a significant proportion of the participants in
our study. Similar reports exist regarding the prevalence of CKD
from the Western world and Asia.
39-41
However, varying reports from the African region exist. In a
recent community survey from Senegal that studied 1 037 adults,
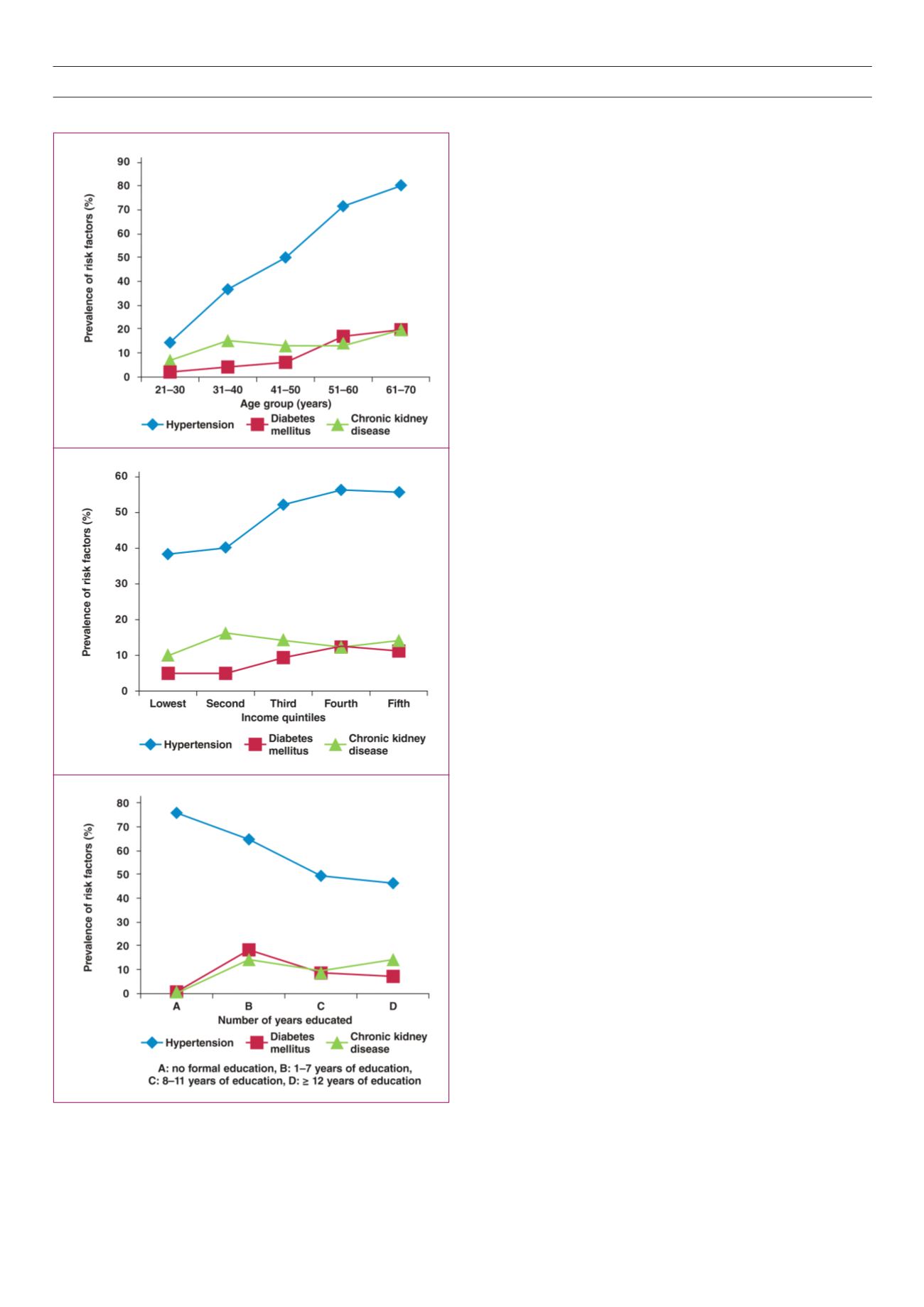
Fig. 2.
Prevalence of non-communicable diseases in relation to some
sociodemographic characteristics among 883 staff members of the
University of Jos.
A
B
C



















