SA JOURNAL OF DIABETES & VASCULAR DISEASE
RESEARCH ARTICLE
VOLUME 13 NUMBER 2 • DECEMBER 2016
71
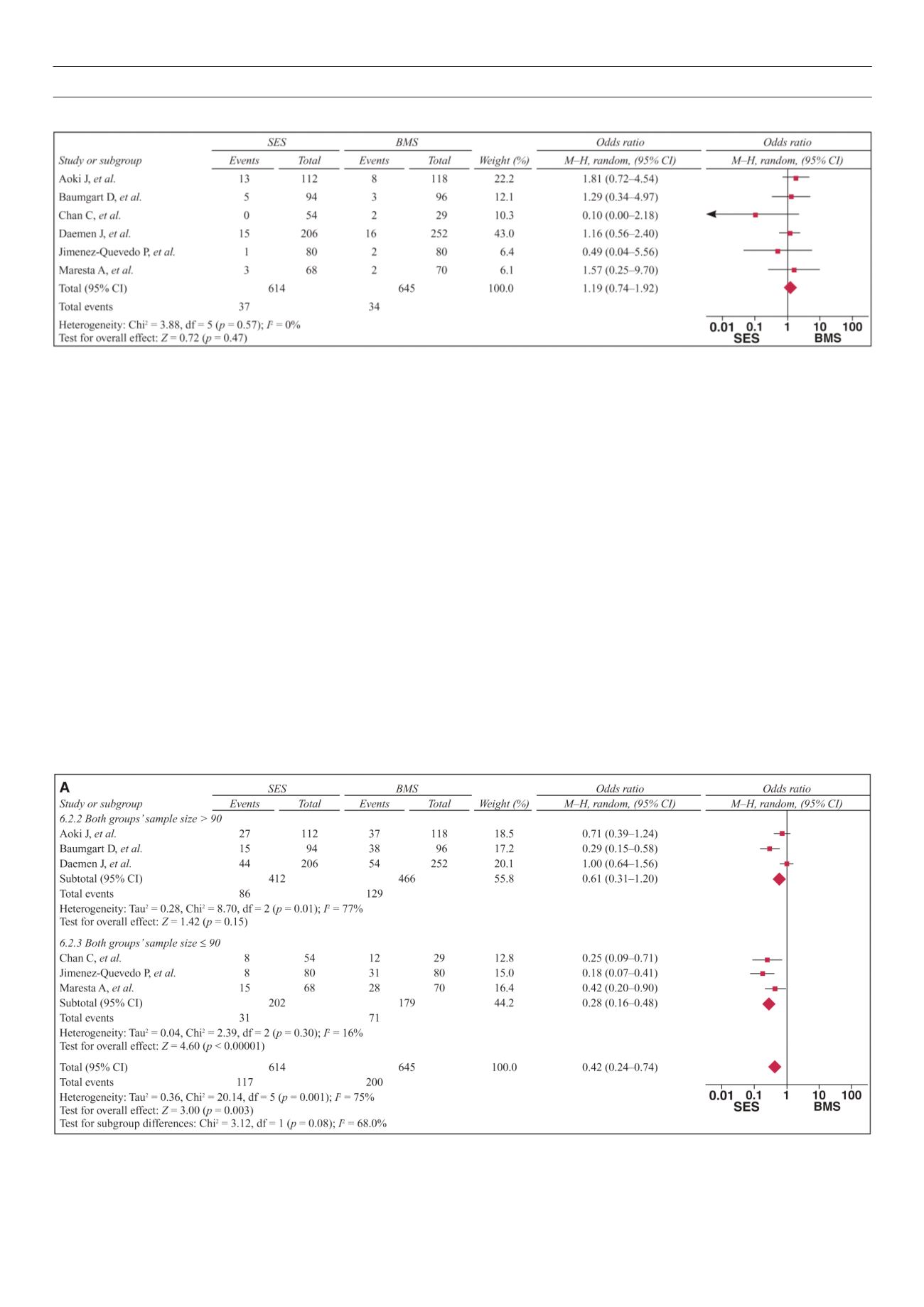
6A–C, the pooled OR was 0.28 (95% CI: 0.16–0.48,
p
< 0.01,
Fig. 6A) for SES versus BMS in studies whose sample size was
above 90, with heterogeneities between the studies (
Q
2
= 8.7,
I
2
= 77%,
p
< 0.1). The pooled OR was 0.61 (95% CI: 0.31–1.21,
p
> 0.05, Fig. 6A) in studies whose sample size was 90 or less,
without heterogeneities between the studies (
Q
2
= 2.39,
I
2
= 16%,
p
> 0.1).
The pooled OR was 0.45 (95%CI = 0.27–0.77,
p
< 0.01, Fig. 6B)
in studies whose subjects were European, without heterogeneities
between the studies (
Q
2
= 3.71,
I
2
= 46%,
p
> 0.1). The pooled OR
was 0.37 (95% CI: 0.11–1.27,
p
> 0.05, Fig. 6B) in studies whose
subjects were American and Asian, with heterogeneities between
the studies (
Q
2
= 15.55,
I
2
= 87%,
p
< 0.1).
The pooled OR was 0.28 (95% CI: 0.19–0.42,
p
< 0.01, Fig. 6C)
in studies whose study method was RCT, without heterogeneities
between the studies (
Q
2
= 2.4,
I
2
= 0%,
p
> 0.1). The pooled OR
was 0.87 (95% CI: 0.61–1.24,
p
> 0.05, Fig. 6C) in studies whose
method of study was non-RCT, without heterogeneities between
the studies (
Q
2
= 0.92,
I
2
= 0%,
p
> 0.1).
By removing one study at a time, a sensitivity analysis was
performed and the model was rerun to determine the effect on
each estimate. It showed that the above meta-analysis estimates
did not change significantly after removal of each study, implying
that these results were statistically reliable.
Discussion
A growing number of studies has shown the efficacy and safety
of SES versus BMS for treating CAD patients with diabetes,
9,29
but
the outcome has been controversial. In this analysis, we retrieved
six studies, which included 1 259 CAD subjects with diabetes, and
performed a meta-analysis. It showed that the SES group had a
significant reduction in major adverse cardiac events, as well as
target-lesion revascularisations, compared with the BMS group.
There was no significant difference for myocardial infarction or
mortality.
These results are consistent with a recent study that suggested
a significant reduction in target-vessel revascularisations with SES,
but with similar mortality rates.
9
Unlike this study, in which the
incidence of myocardial infarction was higher, our analysis showed
no difference for myocardial infarctions between the groups.
Another recent study conducted in Europeans confirmed the
efficacy of SES compared with BMS, along with comparable
Fig. 5.
Forest plots of studies with mortality events in the SES group versus the BMS group.
Fig. 6. A
: Forest plots of sample size subgroups.



















