34
VOLUME 15 NUMBER 1 • JULY 2018
ACHIEVING BEST PRACTICE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
Discussion
Primary healthcare facilities may in most cases be the only available
or accessible form of healthcare for the majority of the population.
2,3
This can be see in the 128 million people who were seen or visited a
PHC clinic in 2013/2014.
23
It is very likely that a significant number
of these patients were diabetic. We know that in Gauteng alone,
740 118 diabetic patients were seen at various PHC clinics for
routine diabetic follow-up visits in 2012/13.
4
However, to date,
there are no data available on the number of diabetic patients who
had a diabetic foot assessment as part of their routine diabetes care
coming from PHC clinics.
Our study has provided evidence of diabetic patients presenting
at PHCs who are at real risk for developing DFU. This develops as
a consequence of a combination of risk factors, most commonly
peripheral neuropathy, peripheral vascular disease, foot deformity
and (unperceived) trauma. In our study, we recorded all these risk
factors in the diabetic patients.
The life-time risk of a diabetic patient developing a DFU is
estimated to be as high as 25%.
24
Therefore early identification
of risk factors that may lead to tissue breakdown is important, as
potential DFU sites are often not diagnosed in diabetic patients
until tissue loss is evident, usually in the form of a non-healing
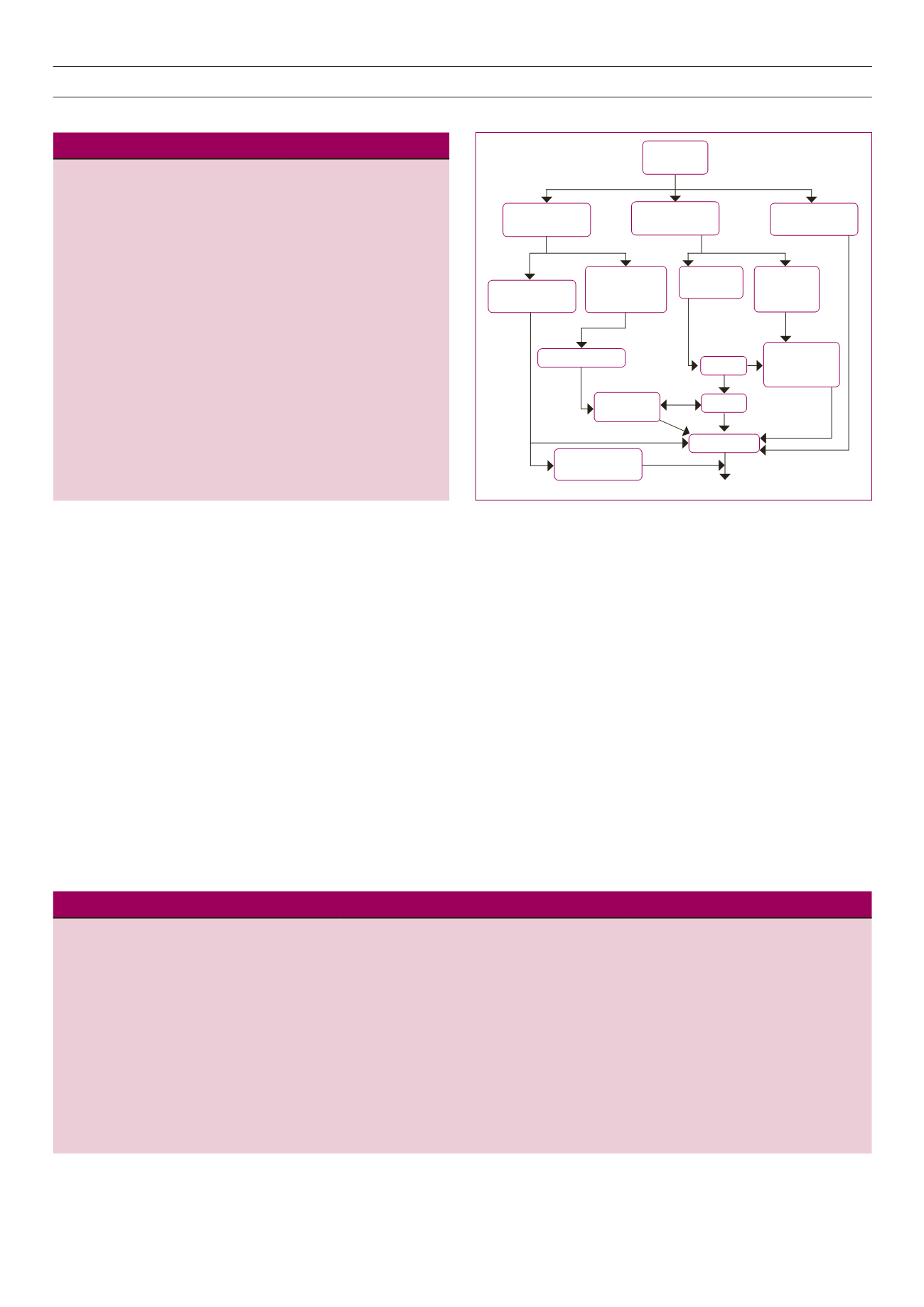
ulcer. Although the DFU pathway (Fig. 3) is a complex multi-
factorial process involving interactions between numerous risk
factors leading to skin breakdown, up to 85% of amputations
could be prevented via routine diabetic foot assessment and early
identification of risk factors.
25,26
Foot assessment and the resultant early identification of those
patients who are at risk for foot ulceration is therefore paramount
in the prevention of DFUs. Early risk identification and regular
inspection of the feet (by podiatrists) has been identified as the
cornerstone in the prevention and management of diabetic foot
complications.
27
The annual diabetic foot inspection has been identified as
probably the single most important tool available in the prevention
of DFUs.
28
The aim of such assessment is to identify those with
early signs of complications and institute appropriate interventions,
such as determining the frequency of clinic visits and actions to
be taken to prevent the progression of risk factors into DFUs. The
Fig. 3.
The pathway to foot ulceration in diabetes. From Boulton
et al
.
38
Table 2.
Foot pathologies and symptoms recorded in diabetic patients
Foot pathology/complaint
Prevalence,
n
(%)
Corns
82 (26)
Calluses
125 (40)
Ulcers/wounds
87 (28)
Infections
79 (25)
Thick nails
13 (4)
Ingrown nail
66 (21)
Fissures/cracks
102 (32)
Interdigital maceration
67 (21)
Burning feet
50 (16)
Tingling
97 (31)
Numbness
89 (28)
Cold feet
70 (22)
Intermittent claudication
54 (17)
Pes planus (flat feet)
98 (31)
Hammer toes
7 (2)
Bunions
22 (7)
Overlapping toes
5 (1)
Pes cavus (high arches)
15 (5)
Table 3.
Components of the diabetic foot examination (adapted from Boulton
et al
.
38
)
Inspection
Neurological
Vascular
Evidence of past/present ulcers
Foot shape
Prominent metatarsal heads/claw toes
Hallux valgus
Muscle wasting
Charcot deformity
Dermatological
Skin status: colour, thickness, dryness, cracking
Sweating
Infection: check between toes for fungal infection
Ulceration
Calluses/blistering: haemorrhage into callus
Erythema
Dystrophic nails
10-g monofilament at four sites on each foot + one of
the following:
Vibration using 128-Hz tuning fork
Pinprick sensation
Ankle reflexes
Vibration perception threshold
Foot pulses
Ankle–brachial index, if indicated
Doppler wave forms, if indicated
Diabetes
Mellitus
Distal sensory
neuropathy
Autonomic
neuropathy
Periphereal
vascular disease
Loss of protective
sensation
Small-muscle
wasting
Muscle atrophy
Loss of
sweating
Increased
peripheral
blood flow
Foot deformities
Dry skin
Distended foot
veins
Warm foot, dry
Increased
foot pressure
Callus
Foot at risk
Repetitive trauma
Unperceived injury
Foot ulcer



















