RESEARCH ARTICLE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
58
VOLUME 16 NUMBER 2 • NOVEMBER 2019
are reported to have reduced NO bioavailability compared to
their Caucasian counterparts.
12,13
Also, Tibetan type 2 diabetes
patients are reported to have less NO levels than their Chinese
Han counterparts.
14
On the other hand, research evidence has also
shown that both tissue and serum AGE levels may be influenced
by genetics.
12,15
Taken together, this information suggests that the
association between serum (and tissue) AGE levels and endothelial
dysfunction may be influenced by the genetic make-up and
ethnicity/race of an individual. However, with the exception of a
single study that investigated the association between serum AGE
levels and endothelial dysfunction among Chinese type 2 diabetes
patients,
16
there is no other information in the literature regarding
the association between serum levels of AGEs and endothelial
dysfunction. In particular, no study has ever been conducted
to investigate the association between serum AGE levels and
endothelial dysfunction among type 2 diabetes patients of black
African descent. Therefore, the aim of this study was to investigate
the association between the different types of serum AGEs and
circulating markers of endothelial dysfunction among black South
African patients with type 2 diabetes mellitus.
Methods
A random sample of 138 black type 2 diabetes patients attending
the diabetes clinic of Dr George Mukhari Academic Hospital
(DGMAH) for medical review, and a convenient sample of 81 age-
matched non-diabetic control subjects were recruited into this study.
The control subjects were recruited mainly from the orthopaedic
wards of DGMAH. Controls were included in the study if they had
fasting blood glucose level of < 6.1 mmol/l. Both type 2 diabetes
patients and control subjects were excluded from the study if they
had any sign of renal impairment, history or evidence of any of
the factors known to affect endothelial dysfunction, such as the
traditional cardiovascular risk factors, uncontrolled hypertension,
dyslipidaemia, cigarette smoking and obesity.
All type 2 diabetes patients and control subjects gave their
informed consent after the purpose of the study and their rights
were clearly explained to them. The study was conducted in
accordance with the requirements of the research and ethics
committee of the University of Limpopo (MREC/P/2013/PG).
After an overnight fast, venous blood samples for measurement
of levels of the different types of serum AGEs, urea and electrolytes,
as well as selected circulating markers of endothelial dysfunction
were collected from all participants into blood collection tubes (BD
Vacutainer
®
, Franklin Lakes, NJ, USA). The samples were left to clot
for 30 min and then centrifuged at 4 000 rpm for 15 min at 4°C.
Aliquots of the resultant serum samples were then stored at –80°C
until analysed. For blood glucose and glycated haemoglobin (HbA
1c
)
measurements, blood samples were collected into citrate and EDTA
blood tubes, respectively.
Serumtotal immunogenicAGEs (TIAGEs),N
e
-carboxymethyllysine
(CML) and N
e
-carboxyethyl-lysine (CEL) were measured using STA-
317, STA-316 and STA-300 OxiselectTM ELISA kits, respectively,
(2BScientific, Upper Heyford, UK), according to the manufacturer’s
instructions. Fluorescent serum AGEs (FAGEs) were measured
according to the method described by Munch
et al
.
17
In brief,
20 μl of serum was diluted to a volume of 10 ml with 20 mM
phosphate buffered saline, pH 7.4. Fluorescence of the diluted
sample was then measured spectrofluorometrically (excitation at
370 nm and emission at 440 nm) using a GloMaxR multidetection
spectrofluorometer (Promega Corp, Madison, WI, USA). Fluorescent
readings were expressed as arbitrary units (emission intensity/
excitation intensity).
Plasminogen activator inhibitor-1 (PAI-1) was measured using
ELISA kits purchased from Cell Biolabs, and NO and endothelin-1
(ET-1) were measured using colorimetric and immunometric kits,
respectively, purchased from Cayman Chemical’s ACE. Fasting blood
glucose levels were measured using a commercially available glucose
oxidase-based kit adapted to the Beckman Coulter
®
UniCell DXC
800 Synchron
®
Clinical System available in the National Laboratory
Health Services (NLHS) laboratory at the DGMAH. HbA
1c
level was
measured using the immune chemiluminescent assay kit adapted
to the Abbot Architect system Ci 8200 in the NLHS laboratory at
DGMAH, in accordance with the manufacturer’s instructions.
Statistical analysis
All analyses were performed using the Statistical Package for the
Social Sciences (SPSS) software (Version 23.0), SPSS Inc, Chicago,
IL, USA. Continuous variables are expressed as mean ± standard
deviation (SD) while categorical variables are expressed as
percentages. Means of the experimental and control groups were
compared using the student’s
t
-test, and
p
< 0.05 was regarded
as statistically significant differences between the groups. Bivariate
logistic regression and the Spearman rank correlation coefficient
were used to determine the association and correlation between the
major types of serum AGEs and circulating markers of endothelial
dysfunction, respectively. Significance level was set at
p
< 0.05.
Results
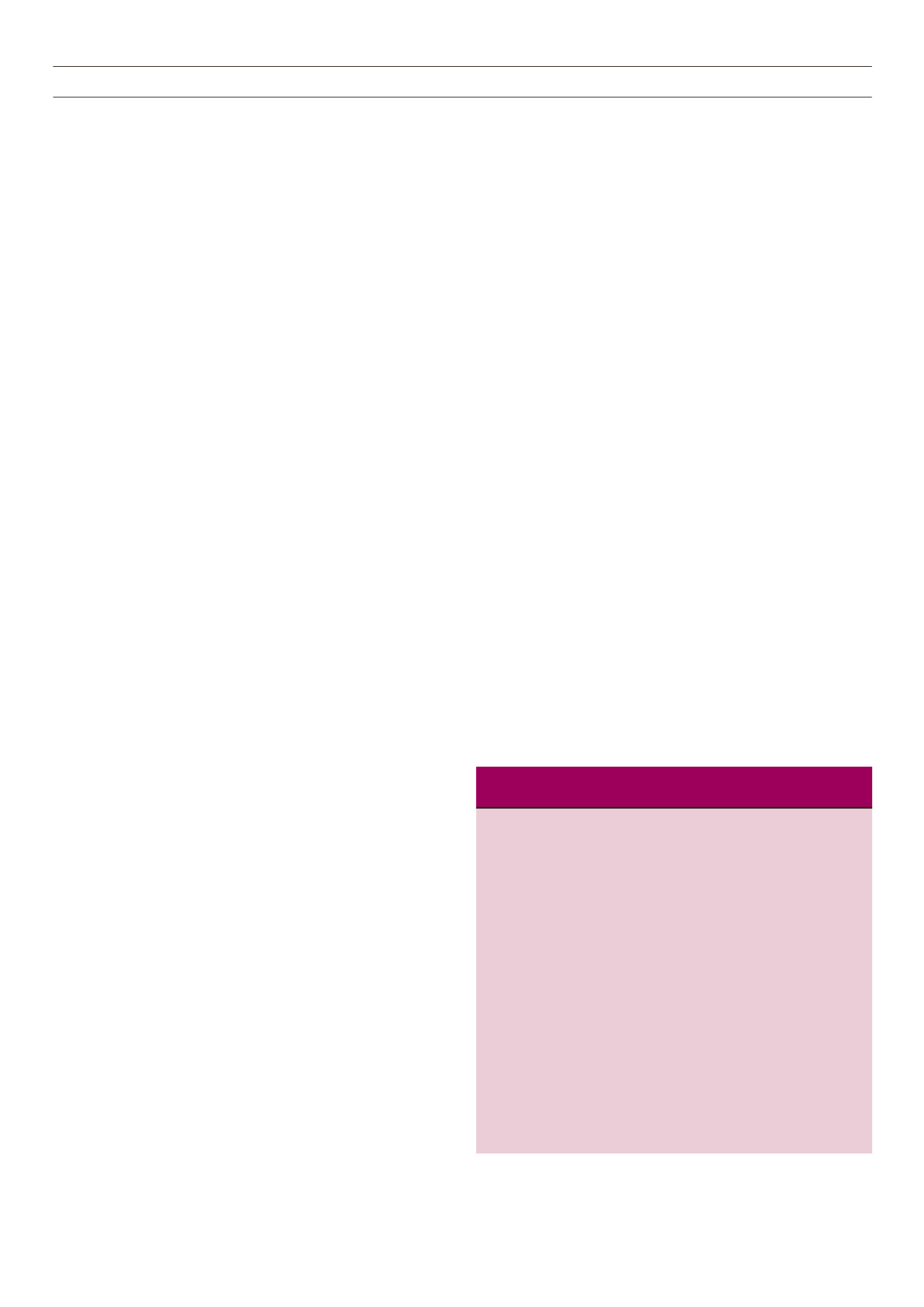
Table1shows thedemographic, clinical and laboratory characteristics
of the type 2 diabetes patients and the non-diabetic controls. With
the exception of the fasting blood glucose and HbA
1c
levels, there
were no significant differences in any other demographic, clinical or
laboratory parameters between the diabetic and the non-diabetic
groups.
Table 1.
Demographic, clinical and laboratory characteristics of the
study subjects
Type 2 diabetes Non-diabetic control
group (
n
= 120)
group (
n
= 83)
Characteristics
mean ± SD
mean ± SD
p
-value
Gender
Male,
n
(%)
49 (41)
36 (44)
0.512
Female,
n
(%)
71 (59)
47 (56)
0.734
Age (years)
56.9 ± 9.4
51.1 ± 9.8
0.152
FBG (mmol/l)
11.6 ± 3.3
5.2 ± 6.3
0.012*
HbA
1c
(%)
9.7 ± 1.2
6.1 ± 2.6
0.037*
HbA
1c
(mmol/mol) 81 ± 0.99
43 ± 5
0.037*
BMI (kg/m²)
26.6 ± 4.7
25.8 ± 5.5
0.081
TC (mmol/l)
4.20 ± 1.80
4.03 ± 0.95
0.174
LDL (mmol/l)
2.3 ± 0.15
2.1 ± 0.2
0.511
TG (mmol/l)
1.2 ± 0.5
1.32 ± 0.4
0.712
SBP (mmHg)
127 ± 10.9
1 28 ± 8.7
0.141
DBP (mmHg)
81 ± 10.8
82 ± 8.4
0.091
Urea (mmol/l)
6.0 ± 2.5
5.6 ± 1.3
0.452
Creatinine (μmol/l) 94 ± 55.9
86.4 ± 21.1
0.318
FBG: fasting blood glucose; HbA
1c
: glycated haemoglobin; BMI: body mass
index; TC: total cholesterol; LDL: low-density lipoprotein; TG: triglycerides;
SBP: systolic blood pressure; DBP: diastolic blood pressure; GFR: glumerular
filtration rate.



















