
SA JOURNAL OF DIABETES & VASCULAR DISEASE
RESEARCH ARTICLE
VOLUME 17 NUMBER 2 • NOVEMBER 2020
45
In patients without a history of DM, raised blood glucose may
correspond to a pre-diabetic state unmasked under a stressful,
acute post-ACS phase. In the GAMI trial, OGTT was systematically
performed in the follow up of 181 patients with acute myocardial
infarction, no history of DM and an admission blood glucose level
< 11.0 mmol/l. This study found 67% of new cases of DM and
impaired glucose intolerance (IGT).
18
The potential mechanisms involved with acute hyperglycaemia
are still poorly understood, but some hypotheses have been
suggested.
4,5
Hyperglycaemia may be a cause or ‘marker’ of
catecholaminergic stress in the post-ACS phase, particularly in
relation to the extent of the infarction and the relative alteration
of LVEF.
19
Evidence of a reduced mortality rate after lowering blood
glucose levels on insulin therapy argues against blood glucose as
a simple epiphenomenon of the stress state.
20
Hyperglycaemia is
associated with insulin resistance, increased levels of free fatty
acids,
21
marked inflammatory response, and endothelial and
microvascular dysfunction, leading to myocardial cell vulnerability,
ischaemia and hypoxia.
22,23
This may explain why in our study,
patients with blood glucose > 140 mg/dl (7.8 mmol/l) had higher
peaks of troponin Ic and cardiac enzymes. Recently, a new concept,
glycaemic variability, has been described in a few studies. In
patients with acute myocardial infarction, glycaemic variability was
associated with the severity of CAD
24
and death.
25
Patients with acute hyperglycaemia and without a history of
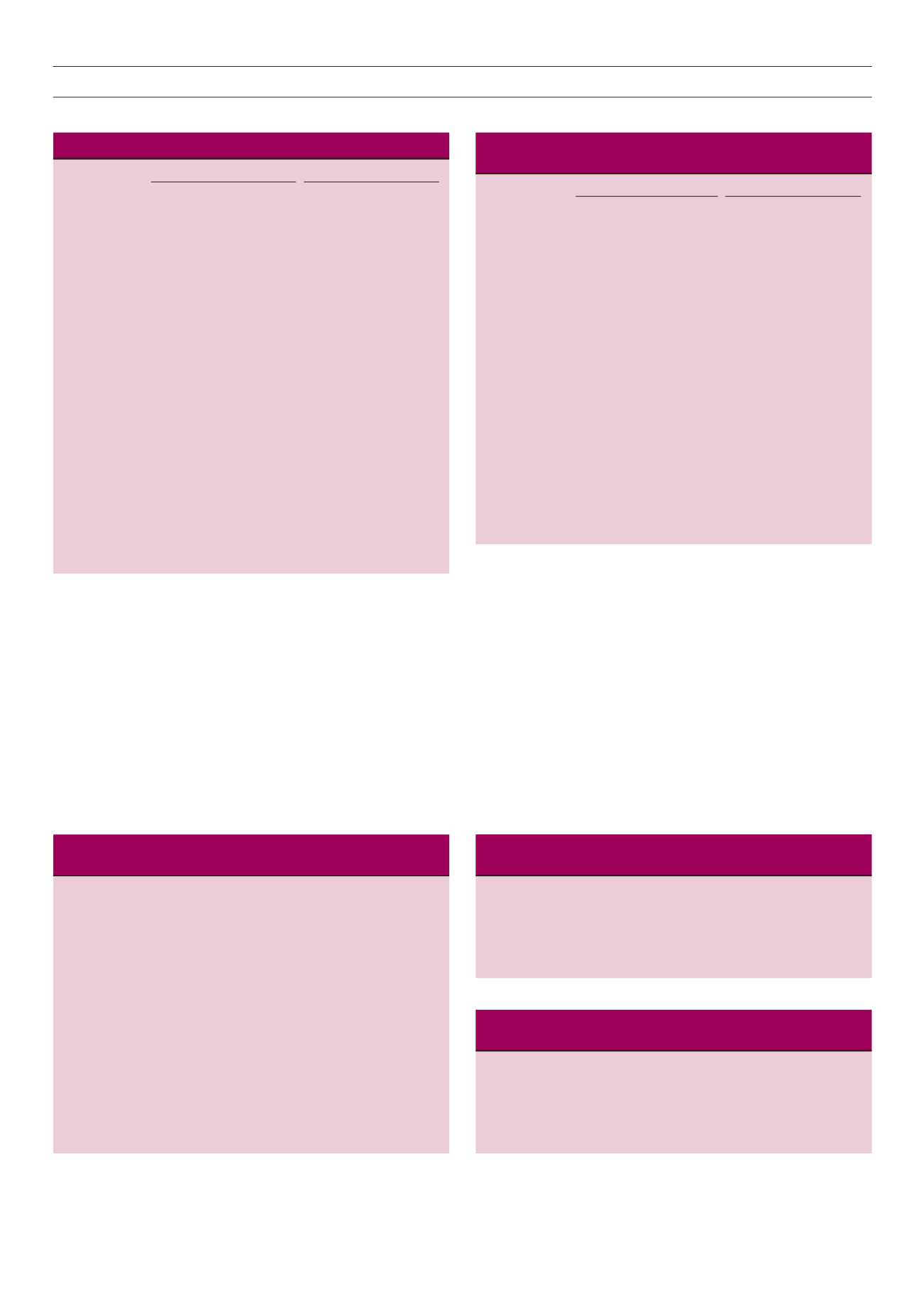
Table 3.
Predictors of in-hospital death. Multivariate analysis
Initial model
Final model
Predictors
HR 95% CI
p
-value HR
95% CI
p
-value
Age > 60 years
1.60 0.95–2.70 0.07
Female gender
0.84 0.47–1.51 0.57
Hypertension
0.88 0.51–1.52 0.65
Diabetes mellitus 1.50 0.85–2.64 0.15
Active smoking
0.53 0.27–1.05 0.57
Dyslipidaemia 0.58 0.32–1.05 0.07 0.48 0.27–0.84
0.01
Admission delay
(hours),
m (IQR)
1.00 0.99–1.01 0.18
Congestive
heart failure
2.25 1.34–3.75 0.002 2.22 1.38–3.56
0.001
LVEF < 40%
6.02 3.37–10.77 < 0.001 6.41 3.72–11.03 < 0.001
Anterior ACS
1.35 0.78–2.35 0.28
Admission
hyperglycaemia 1.76 1.00–3.09 0.05 2.33 1.44–3.77 < 0.001
STEMI
1.75 0.83–3.69 0.14
SVT/VF
3.97 1.47–10.74 0.007 3.43 1.37–8.62
0.008
Cardiogenic
shock
12.32 5.71–26.58 < 0.001 8.82 4.38–17.76 < 0.001
PCI
0.32 0.13–0.80 0.02 0.35 0.16–0.79
0.01
HR: hazard ratio. 95% CI: 95% confidence interval. MI: myocardial infarction.
LVEF: left ventricular ejection fraction. ACS: acute coronary syndrome. STEMI:
ST-segment elevation myocardial infarction. SVT/VF: sustained ventricular
tachycardia/ventricular fibrillation. PCI: percutaneous coronary intervention.
Table 4.
Predictors of in–hospital death in patients with diabetes.
Multivariate analysis.
Initial model
Final model
Predictors
HR 95% CI
p
-value HR
95% CI
p
-value
Dyslipidaemia
0.78 0.28–2.16 0.63
Congestive
6.43 2.12–19.54 0.04 5.74 2.68–12.30 < 0.001
heart failure
LVEF < 40%
1.12 0.42–3.00 0.83
STEMI
1.40 0.36–5.36 0.63
SVT/VF
15.11 1.88–121.20 0.01 10.09 1.41–72.27 0.02
Cardiogenic
29.24 6.83–125.11 < 0.001 23.75 7.60–74.27 < 0.001
shock
DAPT
0.80 0.26–2.41 0.69
PCI
1.07 0.29–3.89 0.92
m (IQR): median (interquartile range). HR: hazard ratio. 95% CI: 95%
confidence interval. LVEF: left ventricular ejection fraction. STEMI: ST-segment
elevation myocardial infarction. SVT/VF: sustained ventricular tachycardia/
ventricular fibrillation. DAPT: dual antiplatelet therapy. PCI: percutaneous
coronary intervention.
Table 5.
Predictors of in-hospital death in patients without diabetes.
Multivariate analysis
Initial model
Final model
Predictors
HR 95% CI
p
-value HR
95% CI
p
-value
Age > 60 years
2.39 1.27–4.49 0.007 2.46 1.35–4.49 0.003
Female gender
0.77 0.37–1.6
0.48
Hypertension
1.17 0.60–2.25 0.65
Dyslipidaemia
0.53 0.24–1.16 0.11
History of MI
0.15 0.02–1.32 0.09
Congestive heart
failure
1.44 0.76–2.74 0.27
LVEF < 40%
8.71 4.05–18.70 0.15 10.18 4.93–21.00 < 0.001
Anterior ACS
1.53 0.78–3.01 0.22
Admission
hyperglycaemia 2.65 1.41–4.99 0.002 3.12 1.72–5.68 < 0.001
STEMI
1.34 0.54–3.30 0.99
SVT/VF
3.59 1.21–10.64 0.021
Cardiogenic shock 7.33 2.81–19.08 < 0.001 9.05 3.66–22.33 < 0.001
PCI
0.27 0.09–0.83 0.022 0.29 0.10–0.86 0.02
HR: hazard ratio. 95% CI: 95% confidence interval. MI: myocardial
infarction.
ACS: acute coronary syndrome. LVEF: left ventricular ejection fraction. ACS:
acute coronary syndrome. STEMI: ST-segment elevation myocardial infarction.
SVT/VF: sustained ventricular tachycardia/ventricular fibrillation. PCI:
percutaneous coronary intervention.
Table 6.
Predictors of in-hospital death from 2002–2010. Multivariate
analysis.
Predictors
HR
95% CI
p
-value
Diabetes mellitus
4.79
1.86–12.36
0.001
Congestive heart failure
4.51
1.74–11.70
0.001
Cardiogenic shock
6.10
1.61–23.05
0.008
HR: hazard ratio. 95% CI: 95% confidence interval.
Table 7.
Predictors of in-hospital death from 2011–2017. Multivariate
analysis.
Predictors
HR
95% CI
p
-value
Admission hyperglycaemia
2.57
1.52–4.32
< 0.001
Congestive heart failure
3.40
2.05–5.64
< 0.001
Cardiogenic shock
14.41
6.82–30.42
< 0.001
HR: hazard ratio. 95% CI: 95% confidence interval.



















