SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 10 NUMBER 3 • SEPTEMBER 2013
97
However, we propose that interim clinical recommendations can
and should be made.
1. Improve the identification of women with PCOS
in primary care
This could be achieved through (i) greater public awareness of PCOS
among women, (ii) increased symptom enquiry by primary care
professionals, and (iii) greater attention given to the investigation
of oligomenorrhoea or hirsutism by simple blood tests. Women
who meet the clinical/biochemical diagnostic criteria for PCOS may
need investigation to exclude other diagnoses, through discussion
with, or referral to an endocrinologist. Most of the differential
diagnoses are relatively uncommon or rare. Differential diagnoses
may be excluded (see table 4) and CMD risk may be determined
through the following investigations (Table 5).
2. Standardisation of the PCOS definition
The identification of women with PCOS, who then could be screened
for type 2 diabetes, would be helped considerably if there were a
universally accepted definition. Current discrepancies between defi-
nitions lead to uncertainty in primary care. Using the NIH classifi-
cation which does not require ultrasound, will result in missing the
diagnosis of some PCOS phenotypes and perpetuating low detection
rates. Yet, even in the UK where the Rotterdam criteria are used to
diagnose this condition, unless women with either oligomenorrhoea
or hyperandrogenism are referred for ultrasound investigation, clini-
cians are essentially basing their diagnosis upon the NIH criteria. It
would be pragmatic therefore to first identify if a woman has hyper-
androgenism and oligomenorrhoea and when only one criteria is
found, to refer for a transvaginal ultrasound to confirm diagnosis.
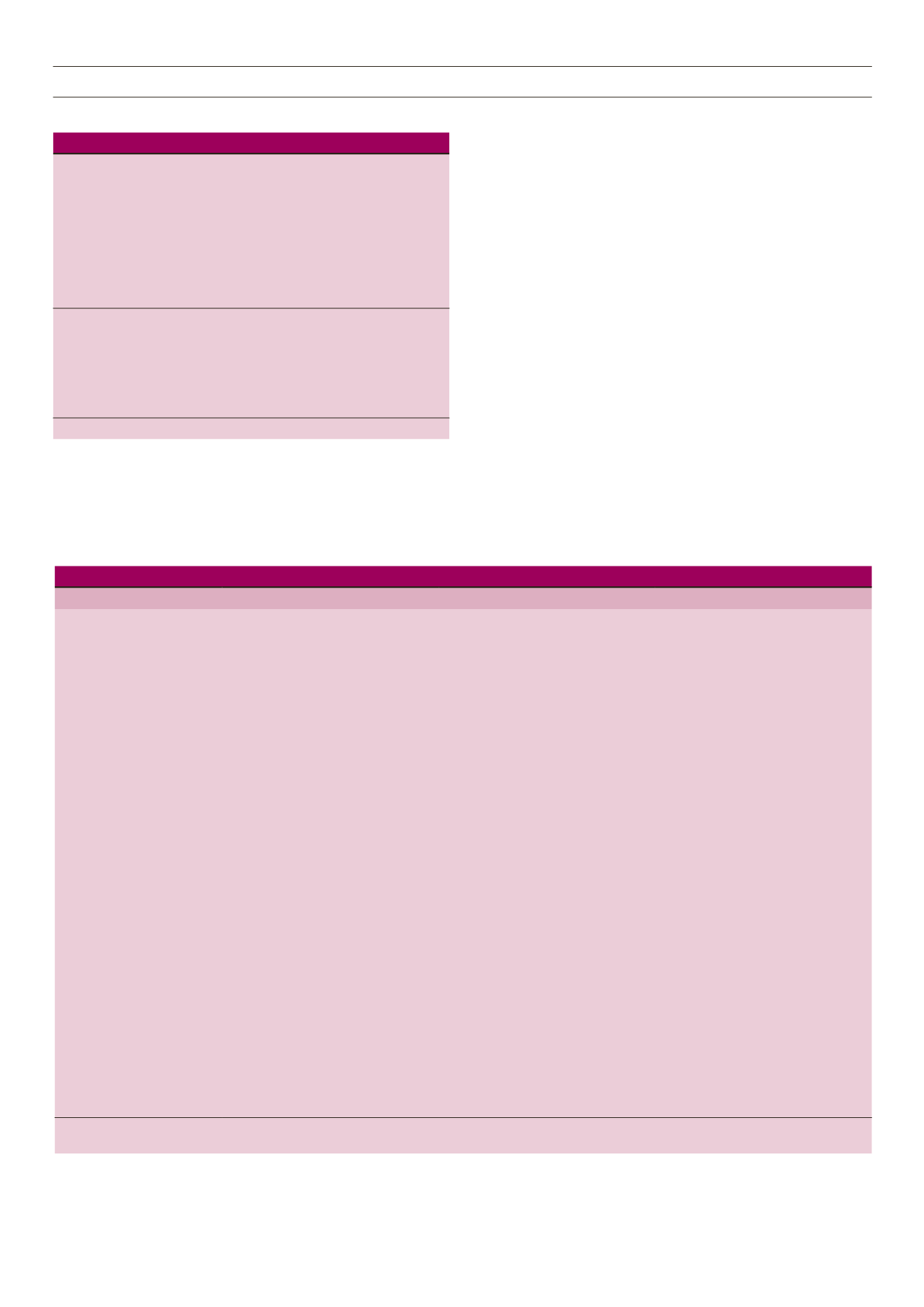
Table 5.
Recommended Investigations for PCOS.
Serum Testosterone or Free Androgen Index
Sex hormone binding globulin (SHBG)
Thyroid stimulating hormone (TSH)
Prolactin
Ultrasound ovaries (transvaginal better than abdominal)
LH and FSH*
17-OH progesterone**
Dehydroepianderosterone sulphate (DHEAS)***
2-hour oral glucose tolerance test****
Lipid profile
*Can be performed as an additional tool to aid diagnosis. PCOS often results
in an increased
LH/FSH ratio. Tests also relevant to exclude other causes of amenorrhoea.
**To exclude congenital adrenal hyperplasia (CAH).
***A second-line measure of adrenal hyperandrogenism.
****HbA
1C
and fasting plasma glucose have not been shown to be
reliable measures for determining abnormal glucose regulation in PCOS.
FSH: follicle stimulating hormone, LH: luteinising hormone.
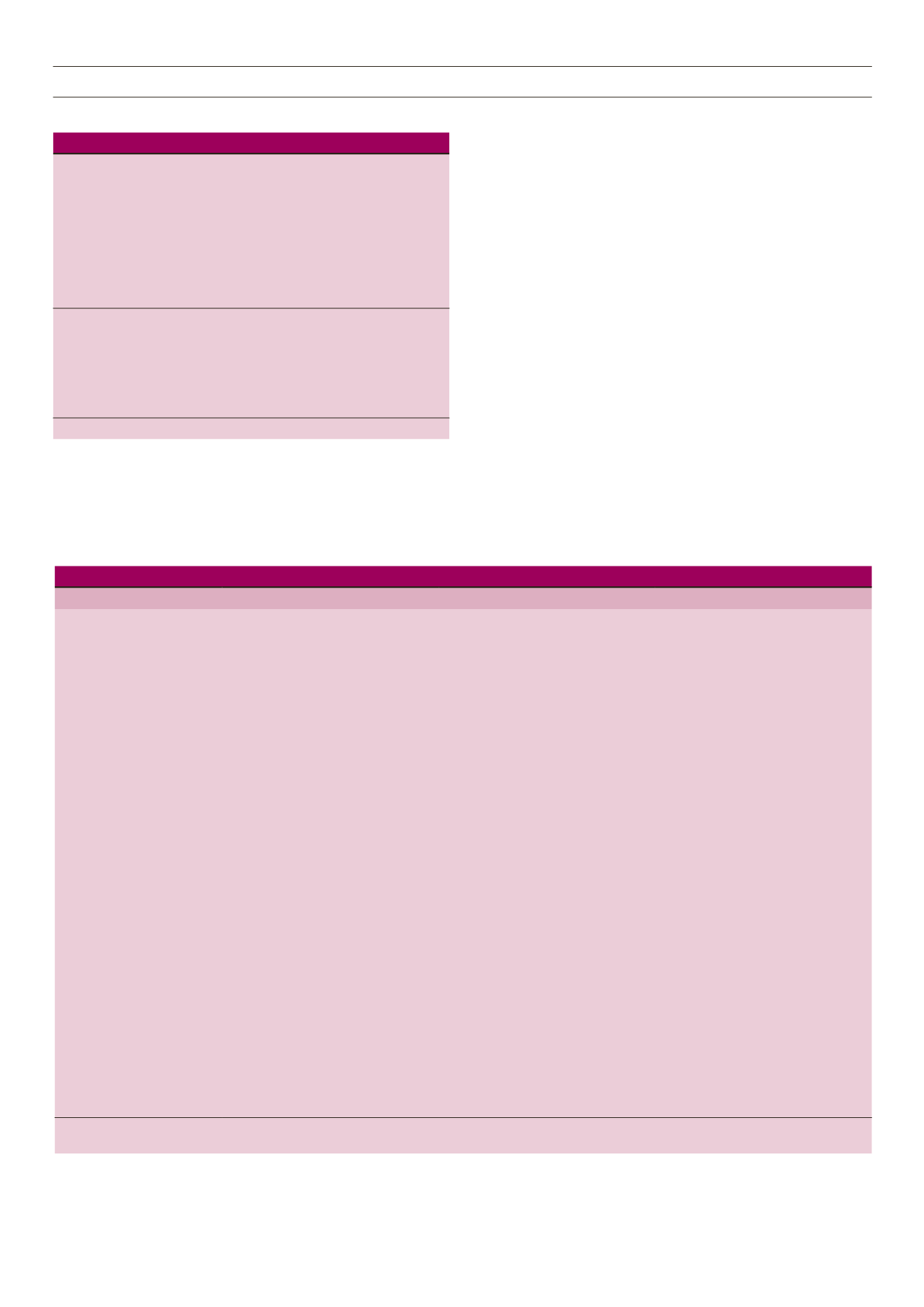
Table 6.
Recommendations for the clinical assessment of CMD in women with PCOS.
Clinical assessment
Recommendation
Minimum frequency
Additional information
Diagnosis
Diagnose by Rotterdam Criteria. Caution
in diagnosis teenagers < 18 years or if
menarche < 2 years ago
Once
Glucose tolerance
2-h oral glucose tolerance test
Every 2 years.
Annually if PCOS and additional
risk factors*
*Additional risk factors:
Increased age, ethnicity, parental history
of diabetes, history hypertension, use of
antihypertensives, smoker, physical in-
activity, increased waist circumference
Cardiovascular risk
Body mass index
(and weight loss advice where
appropriate)
Annually
BMI 18.5–24.9 kg/m
2
= healthy
25–29.9 kg/m
2
= overweight
30+ kg/m
2
= obese
Aim for 5–10% weight loss as initial goal
Waist circumference
Annually
> 80 cm increased metabolic risk
> 88 cm high metabolic risk
Smoking status (advice if smoker)
At each visit
Physical activity status (and advice)
Annually
Recommendation of 150 minutes
physical activity/week
Blood pressure
Annually
Lipid profile
Annually if abnormal or obese. Every
two years if found normal.
Goals:
PCOS only:
• Total cholesterol < 4 mmol/l,
• LDL-C < 3.4, HDL-C > 1.0 triglycer-
ides < 1.7 mmol/l
PCOS and metabolic risk:
• Total cholesterol < 4 mmol/l,
• LDL-C < 1.8–2.6, HDL-C >
1.0,triglycerides < 1.7 mmol/l
PCOS and diabetes:
• Total cholesterol < 4 mmol/l,
• LDL-C < 1.8, HDL-C > 1.0,
triglycerides < 1.7 mmol/l
Adapted from: Teede H
et. al.
(2011) and Fauser
et. al
(2012).
HDL-C: high-density lipoprotein cholesterol, LDL-C: low-density lipoprotein cholesterol.