SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 11 NUMBER 1 • MARCH 2014
17
• One should also remember that HbA
1c
cut-off level makes less
sense for cardiac events because cardiovascular risk depends on
various strong risk factors such as hypertension and smoking
7
(Table 1).
Glucose control in acute coronary syndrome
Elevated plasma glucose level during an acute coronary syndrome
(ACS) is associated with a more serious prognosis in patients
with diabetes than those without. Hyperglycaemia may relate to
previously undetected glucose perturbations but also to stress-
induced catecholamine release, increasing FFA concentrations,
decreased insulin production, and increasing insulin resistance and
glycogenolysis, with a negative impact on myocardial metabolism
and function. Two strategies have been tested in an attempt to
improve prognosis in patients with ACS.
Metabolic modulation
Metabolic modulation by means of glucose–insulin–potassium
(G&K) infusion, regardless of the presence of DM or elevated
plasma glucose levels, is based on the assumption that increase
in intracellular potassium stabilises cardiac myocytes and facilitates
glucose transport into the cell. Other potential benefits include
decreased production of FFA, improved use of glucose for energy
production and improved endothelial function and fibrinolysis.
Despite these proposed mechanistic benefits of glucose,
potassium and insulin therapy, the strategy has been proven futile
in the CREATE trial, which enrolled more than 20 000 patients with
Ml who were randomised to G&K therapy versus usual care. No
benefit of G&K therapy was demonstrated. This lack of effect may
have been due to increased plasma glucose levels or the negative
effect of fluid load induced by G&K infusion.
The DIGAMI trial, which is often misinterpreted as a trial of
intensive glucose control, is actually a glucose–insulin infusion
therapy trial.
8
The first DIGAMI trial randomised 620 patients
with DM and acute myocardial infarction (AMI) to > 24 hours
insulin–glucose infusions, followed by multi-dose insulin, or routine
glucose-lowering therapy.
Mortality after three to four years was significantly reduced
in the intervention group.
8
However DIGAMI-2 failed to replicate
this prognostic benefit. The plausible reason for this discrepancy
was that in DIGAMI-l, admission HbA
lc
levels decreased more
(1.5%) from a higher level (9.1%) compared with 0.5% from
8.3% in DIGAMI-2. Since the DIGAMI-2 trial did not achieve a
difference in glucose control between intensively treated and
control groups, it is still an open question as to whether glucose
lowering is beneficial.
Glucose control in the ICU setting
In 2001, van den Berghe published a randomised, controlled trial
of critically ill surgical patients, showing that tight glucose control
reduced hospital mortality rates.
9
Since the greatest decrease in
death occurred in a subgroup of patients with multi-system organ
failure, it was speculated that the benefits of tight glucose control
might extend to medical ICU patients as well. However, subsequent
trials by the same group could not demonstrate any benefit with
tight glycaemic control.
Further recent trials, such as the VISEP and European glucontrol
showed a trend for increased mortality rate with tight glucose
control. The NICE SUGAR trial in fact demonstrated a 14% increase
in mortality rate with the intensive glucose regimen.
10
Few of these trials assessing glucose control in ICU settings
included ACS patients. Therefore, general applicability of the
observation remains uncertain. Because of a paucity of data on tight
glycaemic control, a glucose target of < l80 mg% is a reasonable
approach in ACS patients.
Why lower is not necessarily better
The UKPDS study was the first to provide evidence that in newly
diagnosed type 2 DM patients, intensive glucose control may reduce
the risk of microvascular complications, also with modest effect on
CV outcomes. Thus the concept ‘the lower, the better’ (glucose
level) was proposed by all diabetology guidelines as a paradigm for
type 2 DM patients. However, this concept has been challenged by
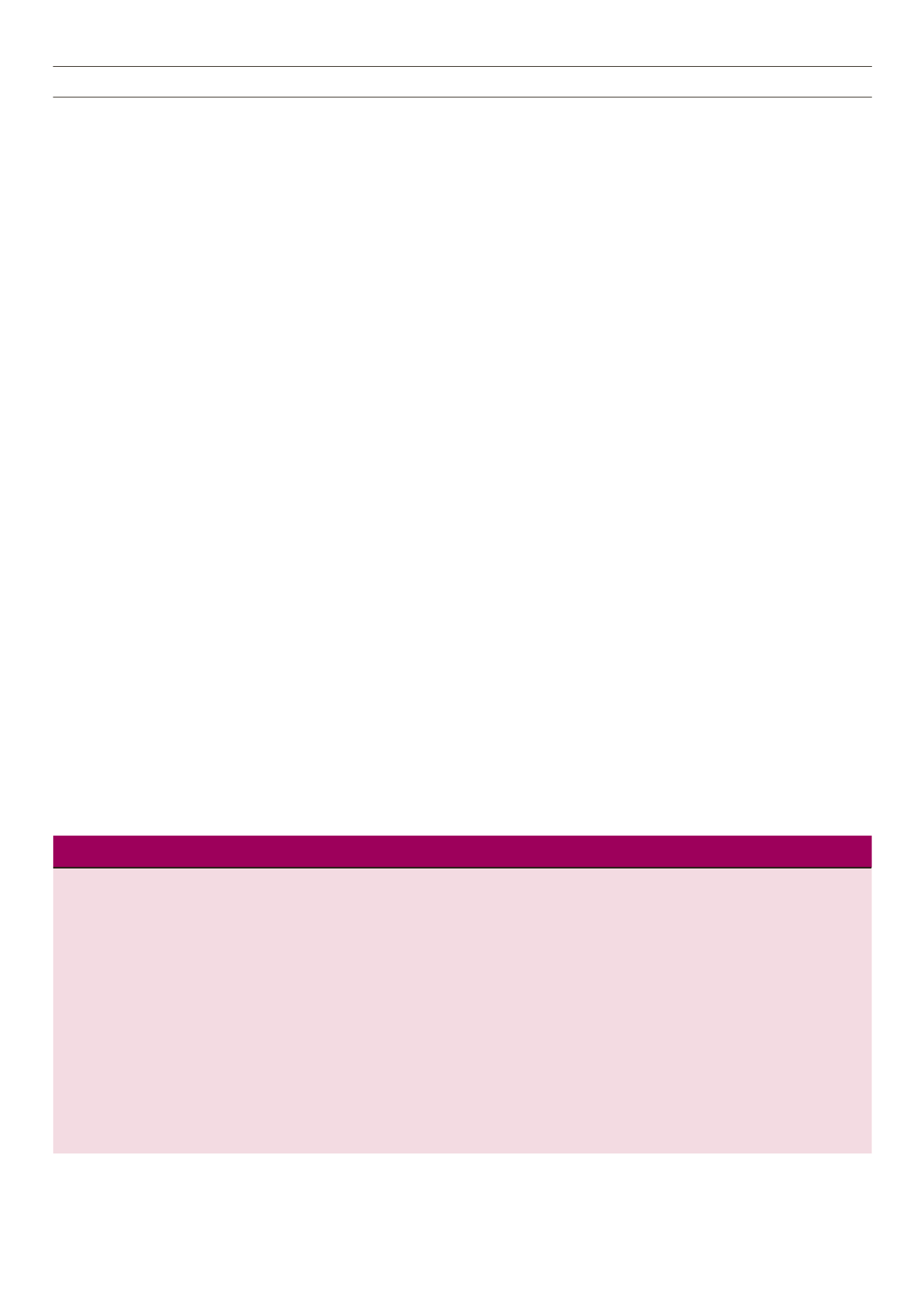
three landmark trials: ACCORD, ADVANCE and VADT.
Numerous potential reasons have been put forward to explain
the lack of benefits with intensive glucose-control therapy. These
include pernicious effects of specific drugs or drug combinations,
increased incidence of hypoglycaemia precipitating CV death, and
ACCORD
ADVANCE
VADT
Number
10 251
11 140
1791
Age (mean, years)
62
66
60
BMI (mean, kg/m
2
)
32
28
31
Follow up (mean, years)
3.5
5
5.6
A
1c
target (%)
< 6.0 vs 7.0–7.9
≤ 6.5 vs standard
< 6% versus 8–9%
Baseline A
1c
(mean, %)
8.3
7.5
9.4%
Endpoint A
1c
(mean, %)
Intensive 6.4 Standard 7.5
Intensive 6.43 Standard 7.0
Intensive 6.9% Standard 8.4%
Severe hypoglycaemic events (%)
Intensive 10.5 Standard 3.5
Intensive 2.7 Standard 1.5
Intensive 8.5% Standard 2.1%
Weight change (kg)
Intensive +3.5 Standard +0.4
Intensive −0.1 Standard −1.0
Intensive +8.1% Standard +4.1%
Major macro- or microvascular event
Not reported
0.9 (0.82−0.98),
p
= 0.01
0.88 (0.74–1.05),
p
= 0.14
Non-fatal MI/stroke, CV death
HR 0.9 (0.78−1.04),
p
= 0.16
0.94 (0.84−1.06),
p
= 0.32
Not reported
All-cause mortality
HR 1.22 (1.01−1.46),
p
= 0.04
0.93 (0.83−1.06),
p
= 0.28
1.07 (0.81–1.42),
p
= 0.62
Non-fatal MI
HR 0.76 (0.62−0.92),
p
= 0.004
0.98 (0.77−1.22),
p
= NS
0.82 (059–1.14),
p
= 0.24
ACCORD: Action to Control Cardiovascular Risk in Diabetes trial; ADVANCE: Action in Diabetes and Vascular disease: preterAx and diamicroN-MR Controlled
Evaluation trial; A
1c
: glycosylated haemoglobin; BMI: body mass index; CV: cardiovascular; MI: myocardial infarction; VADT: Veterans Affairs Diabetes Trial.
Table 1.
Baseline characteristics of the ACCORD, ADVANCE and VADT trials.