VOLUME 11 NUMBER 1 • MARCH 2014
27
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
Glucagon-like peptide-1-based therapies: effects beyond
blood glucose control
Subash C Sivaraman, Thomas M Barber, Paul O’Hare, Harpal S Randeva
Abstract
Therapies based on the gut-derived glucagon-like peptide-1
(GLP-1) are a recent addition to the treatment of type 2
diabetes. They are either inhibitors of the enzyme di-peptidyl
peptidase 4 (DPP-4), which inactivates GLP-1, or analogues
of GLP-1 that are resistant to enzymatic degradation. Clinical
trials show that long-term treatment with these classes of
drugs have a favourable impact on the patient’s lipid profile,
reduce systolic blood pressure and reduce abdominal obesity,
suggesting a significant cardiovascular benefit in addition to
glycaemic control.
Transient nausea and vomiting are common adverse effects
with this class of drugs and may occur due to reduction in
gastric motility. GLP-1 based drugs might be associated with a
slight increase in the risk of acute pancreatitis, but there is no
evidence that these drugs cause pancreatic cancer in humans.
GLP-1 based therapy induces medullary thyroid cancer in rat
models, but there is no evidence of it increasing the risk in
humans.
In animal models, GLP-1 and its analogues improve
markers of diabetic nephropathy and diabetic neuropathy by
modulating inflammatorypathways. Ina ratmodel of diabetes,
GLP-1 analogues preserve pancreatic beta-cell function and
beta-cell mass. On-going studies are investigating whether
these benefits are replicated in humans.
GLP-1baseddrugshaveafavourableeffectoncardiovascular
risk factors. They should be used with caution in patients at
risk of pancreatitis. Animal studies suggest improvement in
microvascular complications of diabetes.
Keywords:
beta-cells, blood pressure, cardiovascular effects,
diabetes, diabetes drugs, glucagon-like peptide 1, inflammation,
microvascular complications, obesity, pancreatic function,
pancreatitis
Introduction
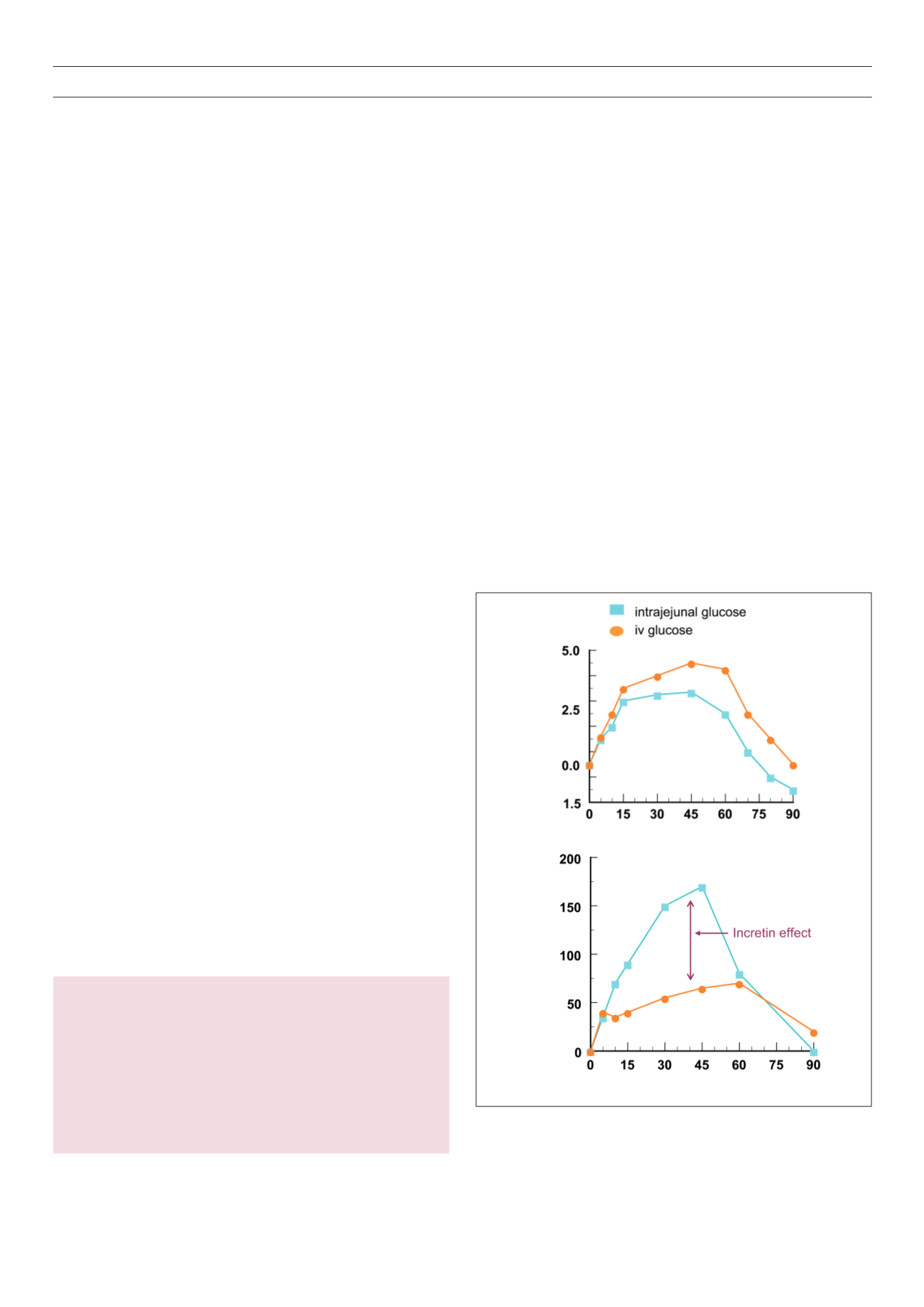
Oral administration of glucose in healthy subjects causes a two-
to three-fold larger insulin response compared to intravenous
administration (Fig. 1). This ‘incretin effect’ is mediated by gut-
Correspondence to: Harpal Singh Randeva
Division of Metabolic and Vascular Health, University of Warwick
Medical School, Coventry, UK
Warwickshire Institute for the Study of Diabetes, Endocrinology
and Metabolism (WISDEM), University Hospitals of Coventry and
Warwickshire (UHCW), NHS Trust, Coventry, UK
e-mail:
Previously published in:
Br J Diabetes Vasc Dis
2013;
13
(5–6): 229–237
S Afr J Diabetes Vasc Dis
2014;
11
: 27–32
derived hormones, of which GLP-1 and glucose-dependent
insulinotropic polypeptide (GIP) are the most important.
1
The
incretin effect depends on the amount of glucose ingested, thereby
keeping blood glucose levels stable in spite of an increased oral
glucose load.
2
The effect of the two hormones, GLP-1 and GIP, is
additive in humans and almost completely explains the incremental
insulin output from the pancreas;
3,4
however, the effect of GLP-1
predominates at higher plasma glucose levels.
5
Both hormones have
a short half-life (2–3 minutes for GLP-1 and 5–6 minutes for GIP)
and are cleared from circulating blood largely by the ubiquitous
enzyme di-peptidyl peptidase 4 (DPP-4)
.6
The gut is the largest endocrine organ in the body: It releases at
least 20 hormonally active peptides with effects on diverse aspects of
energy homeostasis and food intake.
7
GIP, the first incretin hormone
to be isolated, seems to have a greater influence on obesity than
on type 2 diabetes.
8
The predominant action of GLP-2 (which is
structurally similar to GLP-1) is to increase proliferation of epithelial
cells in the small and large bowels.
9–11
The roles of the different
Figure 1.
Insulin secretion in response to intrajejunal and intravenous
administration of glucose. Based on McIntyre
et al
.
Lancet
1964;
2
: 20–21.
Source: reproduced with permission from
Br J Diabetes Vasc Dis
.15
Time (min)
Change from baseline
Insulin (mU/l)
Change from baseline
Glucose (mU/l)
Time (min)