SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 11 NUMBER 1 • MARCH 2014
39
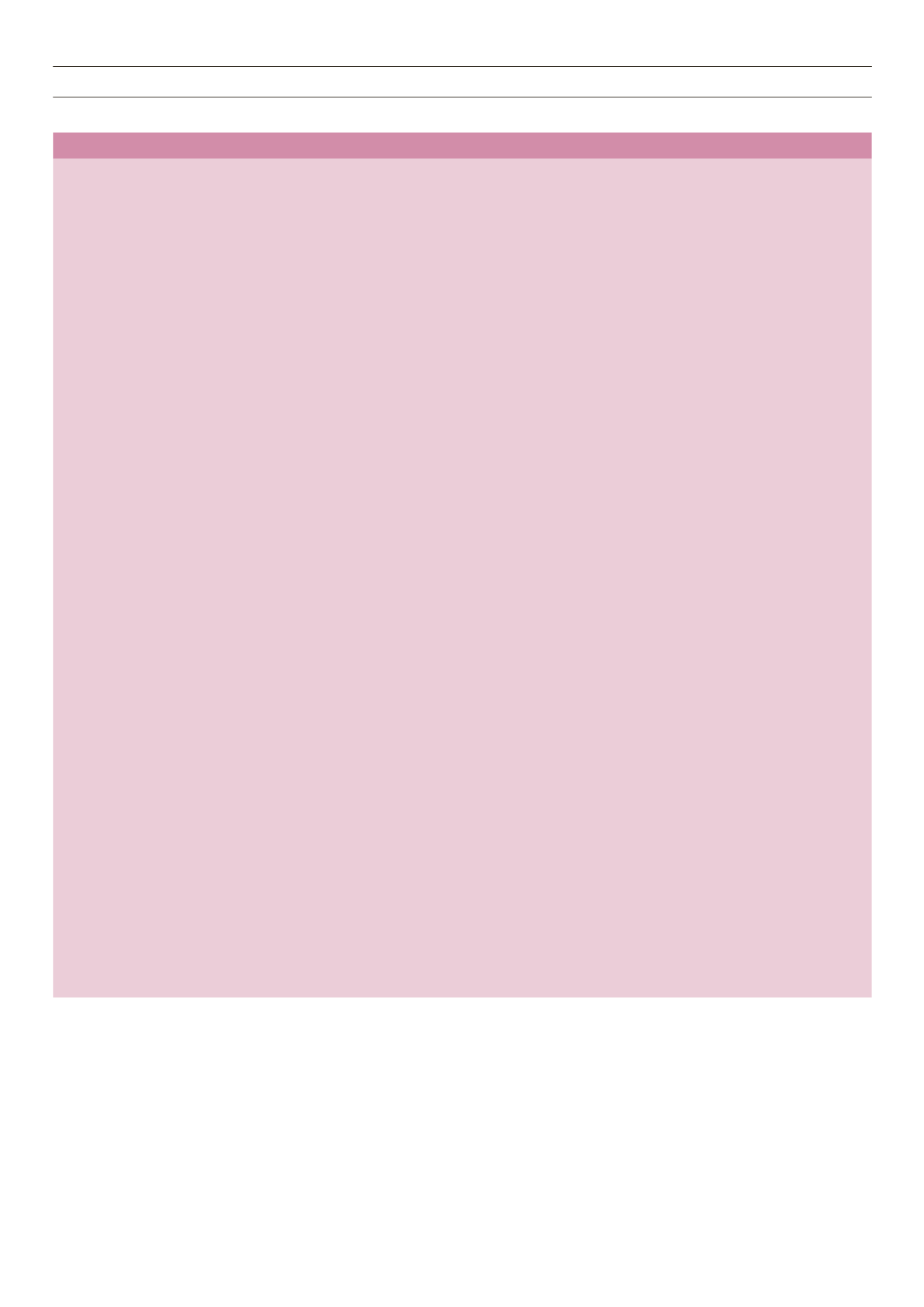
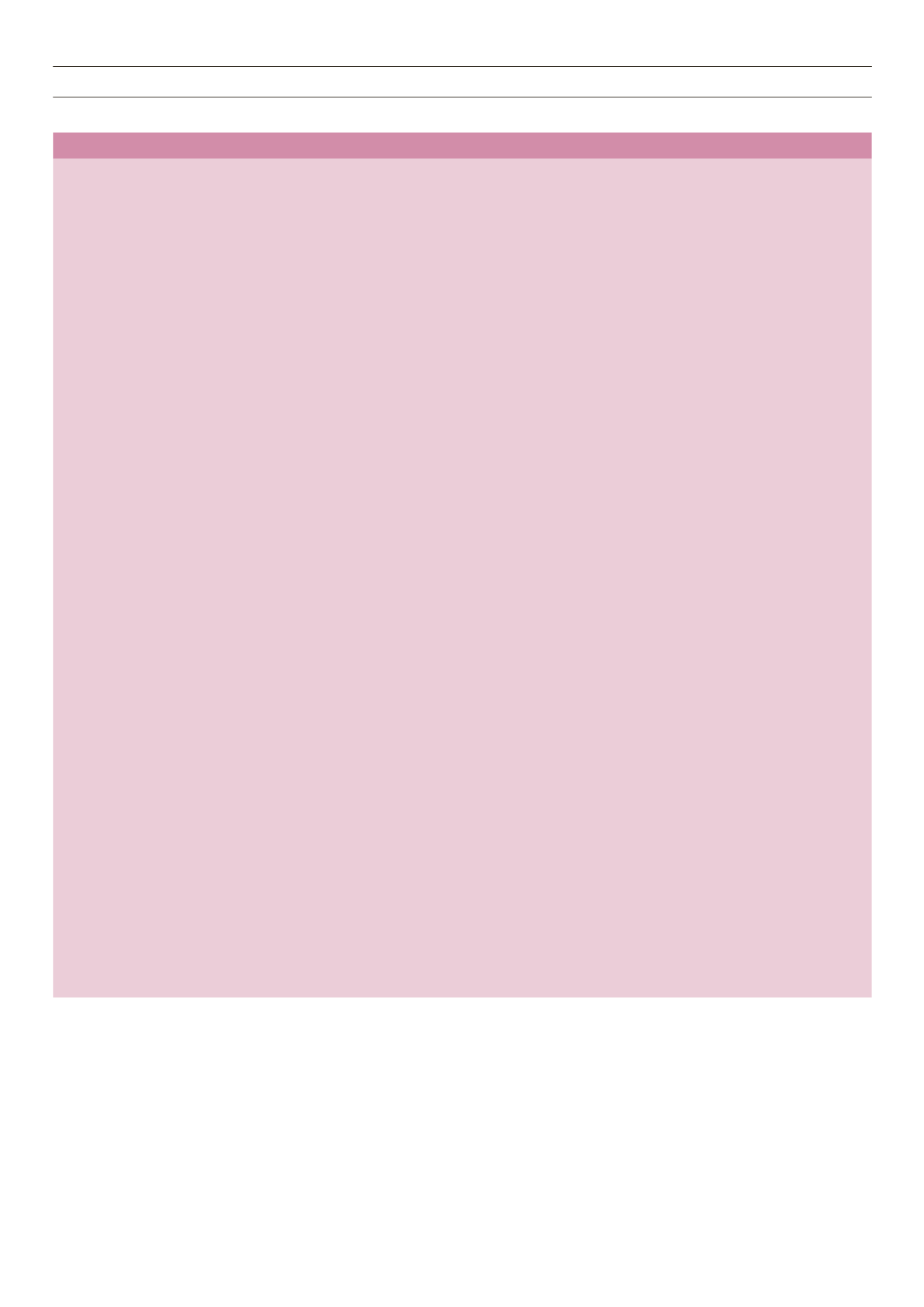
Table 1
. Continued
Types of infection
Antibiotics used
Duration
Other comments
NV infective endocarditis
40,47
MSSA
MRSA
(vancomycin MIC ≤ 2 mg/l)
MRSA
(vancomycin MIC > 2 mg/l,
daptomycin MIC ≤ 1 mg/l)
PV infective endocarditis
40,47
MSSA
MRSA
(vancomycin MIC
≤ 2 mg/l)
MRSA
(vancomycin MIC > 2 mg/l,
daptomycin MIC ≤ 1 mg/l)
Pneumonia
MSSA
MRSA
PVL
S aureus
(necrotising
pneumonia )
Complicated urinary tract
infections
MSSA
MRSA
Eye and CNS infections
MSSA
MRSA
Flucloxacillin 2 g 4–6 h iv
Vancomycin iv aiming for trough
levels of 15–20 mg/l and rifampicin
300–600 mg 12 h po
Daptomycin 6 mg/kg 24 h iv and
rifampicin 300–600 mg 12 h po OR
gentamicin 1 mg/kg iv 12 h
Flucloxacillin 2 g 4–6 h iv, and
rifampicin 300–600 mg 12 h po and
gentamicin 1 mg/kg iv 12 h.
Vancomycin iv aiming for trough
levels of 15–20 mg/l and rifampicin
300–600 mg 12 h po and gentamicin
1 mg/kg iv 12 h.
Daptomycin 6 mg/kg 24 h iv and
rifampicin 300–600 mg 12 h po and
gentamicin 1 mg/kg iv 12 h
Flucloxacillin 1–2 g 6 h iv
Vancomycin iv aiming for trough levels
of 15–20 mg/l OR linezolid 600 mg
12 h iv/po
Linezolid 600 mg 12 h and
clindamycin 1.2 g 6 h iv and if severe
disease e.g. TSS add rifampicin
600 mg bd ± IVIG 2 g/kg.
Flucloxacillin 1–2 g 6 h iv
Vancomycin iv aiming for trough levels
of 15–20 mg/l
Daptomycin could be considered
54
Flucloxacillin 2 g 6 h iv
Vancomycin iv aiming for trough levels
of 15–20 mg/l
Consider adding rifampicin 300–
450 mg 12 h orally to vancomycin
62
4 weeks
4 weeks
4 weeks
6 weeks
6 weeks
6 weeks
10–14 days
14 days for
pyelonephritis.
Abscesses may require a
longer course.
Use 4-h regimen if weight > 85 kg
Use for vancomycin, rifampicin-susceptible
S aureus
strains or when known penicillin allergy. Use lower dose
of rifampicin if creatinine clearance < 30 ml/min
Use for vancomycin-resistant daptomycin-susceptible
S
aureus
strains or patient unable to tolerate vancomycin.
Monitor CPK weekly ans adjust daptomycin dose
according to renal function.
Ensure
S aureus
rifampicin susceptible.
Continue gentamicin for the full course if there are no
signs or symptoms of toxicity
Monitor CPK weekly and adjust daptomycin dose
according to renal function.
Refer to text for surgical interventions
Exclude complicating issues
(e.g. abscess, empyema)
Suspect PVL
S aureus
pneumonia when patient presents
with haemoptysis, hypotension leucopenia, raised CK
level and CXR showing multilobular infiltrates, usually
accompanied by effusions and later cavitation.
12
Catheter change should be undertaken for patients with
long-term urinary catheters.
Patients with peri-nephric or intra-renal abscesses may
require radiology guided or surgical drainage.
There is insufficient evidence to make specific
recommendations in deep eye and CNS infection.
54
The limited data suggest that linezolid may be considered
for the treatment of patients with meningeal or cerebral
infections.
54,90
Intrathecal vancomycin could be considered for CNS
infections.
Acute endophthalmitis is a vision threatening medical
emergency. Patients should be referred to the
ophthalmologists for intravitreal antibiotics and to be
considered for vitrectomy.
62
Key:
bd: twice daily; CK: creatinine kinase; CNS: central nervous system; CXR: chest X-ray; iv: intravenous; IVIG: intravenous immunoglobulin; MRSA: methicillin-
resistant
S aureus
; MSSA: methicillin-sensitive
S aureus
; OPAT: out-patient parenteral antibiotic therapy; MIC: minimum inhibitory concentration; NV: native valve; po:
orally; PVL: Panton-Valentine leukocidin; THA: total hip arthroplasty; TKA: total knee arthroplasty; TSS: toxic shock syndrome.
Most PVL
S aureus
strains in theUK are susceptible to flucloxacillin,
erythromycin and clindamycin. For severe infections, where PVL
S
aureus
(MSSA or MRSA) is suspected with features of toxic shock,
necrotising fasciitis, necrotising pneumonia or purpura fulminans
there may be a theoretical case for using two or three agents.
Health Protection Agency (HPA) guidance recommends linezolid
combined with clindamycin and rifampicin. This is based on
in vitro
synergy and the ability of linezolid and clindamycin to switch off
toxin production.
12,77
Intravenous flucloxacillin is not recommended
for necrotising pneumonia, even in combinations with agents