34
VOLUME 11 NUMBER 1 • MARCH 2014
REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
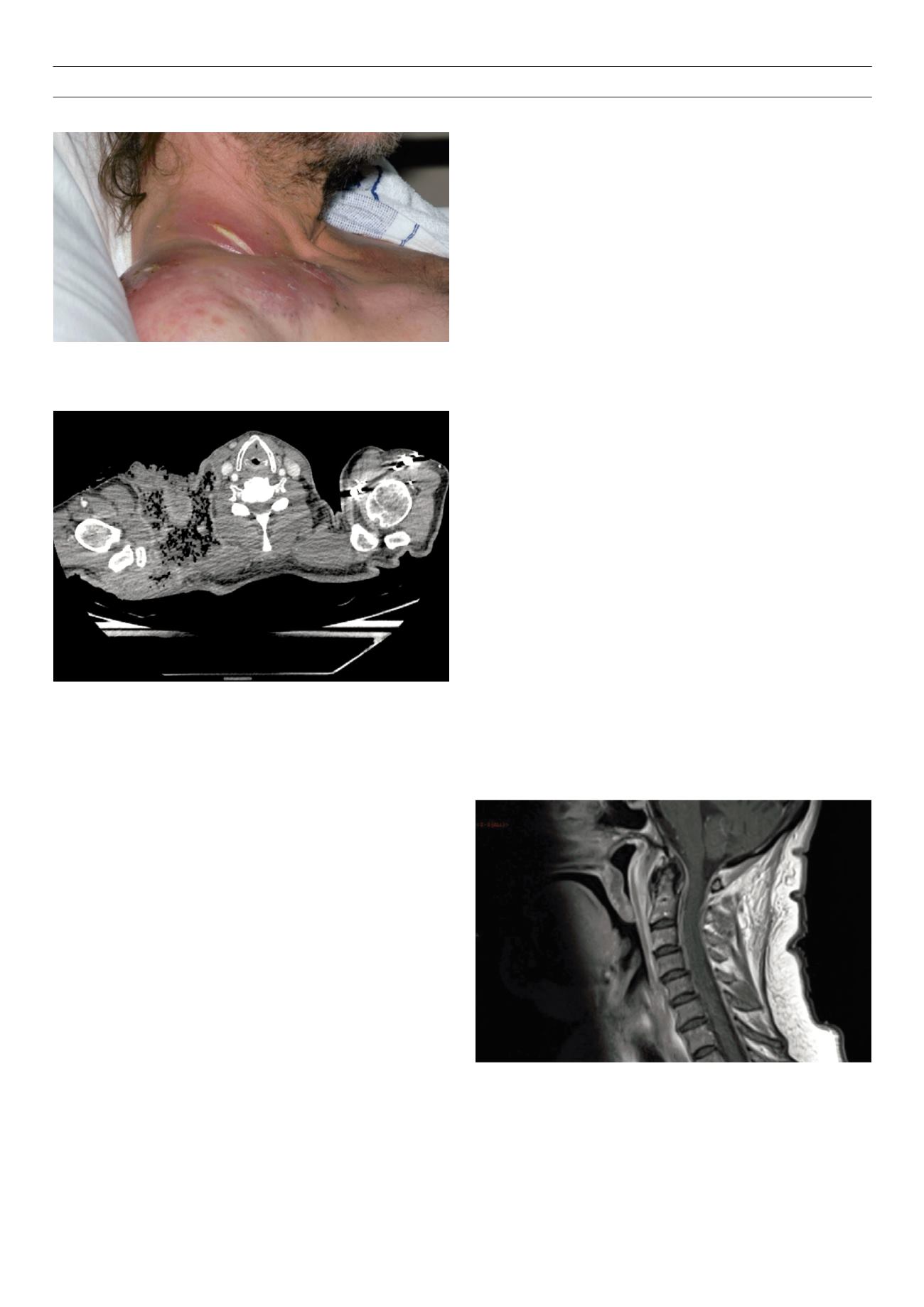
pyogenic staphylococcal infections include impetigo, folliculitis,
furuncles and carbuncles. Carbuncles occur when furuncles
coalesce and extend into deeper subcutaneous tissue (Figs 1a, 1b).
Multiple sinus tracts are usually present and patients may present
with rigors, indicating systemic spread via bacteraemia. Limb
ischaemia and tissue necrosis due to peripheral vascular disease can
complicate SSTIs in diabetic patients.
PVL appears to be a marker for severity and recurrence.
21–23
Like
other
S aureus
strains, PVL
S aureus
strains predominantly cause
SSTI, but can also cause invasive infection. The most serious of these
is a necrotising haemorrhagic pneumonia with a high mortality
rate. The other invasive infections include necrotising fasciitis,
osteomyelitis, septic arthritis, pyomyositis and purpura fulminans.
12
Patients with diabetes are known to be at high risk of
S aureus
BSI and associated complications.
2,24
Traditionally,
S aureus
blood
stream infections (BSIs) are classified according to the environment
of acquisition (healthcare-associated or community-acquired BSI)
and by the absence or presence of identified associated sites of
infection (primary or secondary BSI). Primary BSI accounts for
40–50% of cases of
S aureus
bacteraemia and occurs much less
frequently in patients with healthcare associated bacteraemia
(3–5%) than it does in patients with community acquired
bacteremia.
2,25,26
Infections frequently associated with secondary
BSIs include infective endocarditis (IE), deep-seated abscesses, and
osteomyelitis. In the hospital setting, wound infection and vascular
line- or catheter-related infection are the most common sources of
secondary bacteraemia.
27
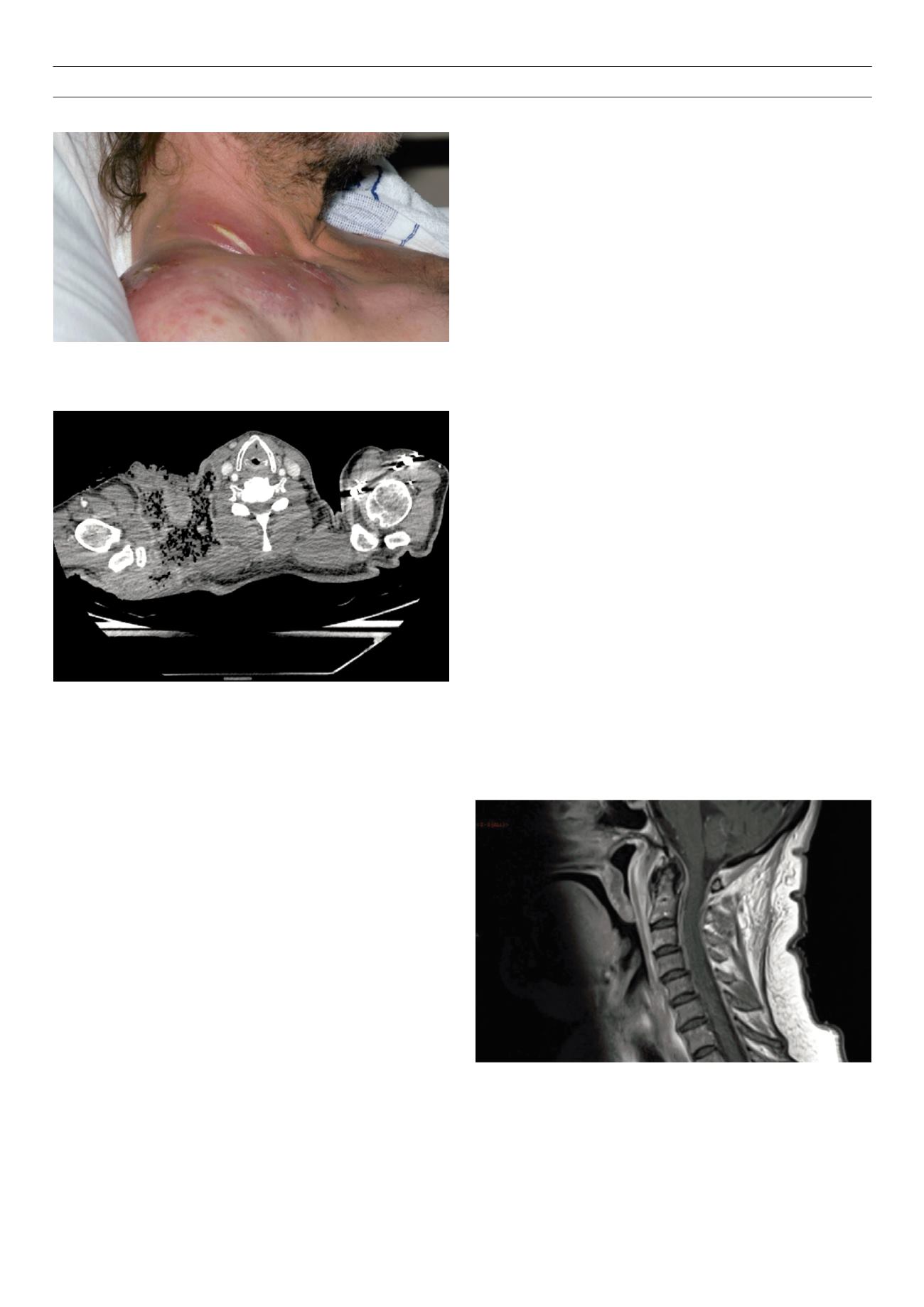
Approximately one-third of patients with
S aureus
BSI develop
local complications or distant septic metastases.
2,28,29
Frequent
sites of distant metastases include the bones and joints (especially
when prosthetic materials are present), the epidural space and
intervertebral discs (Figs. 2 and 3), and both native and prosthetic
cardiac valves (Fig. 4). In addition, patients can develop visceral
abscesses in the spleen and kidneys.
IE is one of the most severe complications of
S aureus
BSI
(Fig. 2).
S aureus
is currently the commonest aetiological agent for
all types of IE, highlighting its ability to infect native valves, even
those that are structurally normal.
2
Approximately half of all patients
with cardiac rhythm management devices or prosthetic valves who
develop
S aureus
BSI will have cardiac device infection.
30–32
The
ability of
S aureus
to form biofilms, makes these infections difficult
to treat without complete surgical removal of the device.
30–32
Overall,
the prognosis of
S aureus
IE is poorer when there are associated
complications that preclude valve replacement surgery (e.g.
persistent bacteraemia, embolic events, and multi-organ failure) or
when the patient has non-IE-related co-morbidities. Similarly, MRSA
IE is associated with a worse prognosis than MSSA IE.
2,8,33
Spondylodiscitis is a term encompassing vertebral osteomyelitis,
spondylitis and discitis (Fig. 3).
S aureus
is the predominant
pathogen, accounting for about half of non-tuberculous cases of
spondylodiscitis.
S aureus
can infect the spine via three routes: by
haematogenous spread, by direct external inoculation as in the case
of trauma or surgery, or by spread from contiguous tissues. The
haematogenous route is predominant, allowing seeding of infection
from distant sites onto the vertebral column. Unlike in children,
the disc is avascular in adults and the intra-osseous anastomoses
involute by the third decade of life, effectively creating end arteries.
This increases the likelihood of a septic embolus resulting in a large
infarct.
34,35
Subsequent spread of infection to the neighbouring disc
and vertebra creates the characteristic lesion of spondylodiscitis.
36
Extensive infarction leads to wedging, cavitation and compression
fractures with resulting spinal instability, deformity and risk of cord
Figure 1a.
Case of Staphylococus aureus carbuncle involving the cervical region
spreading to involve the pectoral region in a patient with type 2 diabetes. Patient
required surgical debridement and 3 months of flucloxacillin therapy.
Figure 1b.
Computed tomography scan showing the extent of the infection
with gas in the subcutaneous tissues involving the right side of neck, supra- and
infraclavicular regions, right axilla and suprascapular regions.
Figure 2.
Magnetic resonance image (MRI) of cervical spine of a patient with type
2 diabetes and fibromyalgia presenting with neck pain.
S aureus
was isolated on
blood cultures and the MRI showed extensive deep infection in the pre- and
para-vertebral tissues, centred at the C1 and 2 levels, extending into the spinal
canal. She was treated with intravenous flucloxacillin followed by teicoplanin as
out-patient parenteral antimicrobial therapy.