SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
VOLUME 11 NUMBER 1 • MARCH 2014
35
compression. Uncontrolled infection can breach the bone and
track into surrounding soft tissues, causing paravertebral or psoas
abscesses, and spread posteriorly into the spinal canal, forming an
epidural abscess with further risk of paraplegia, subdural abscess
and meningitis.
34
Osteomyelitis and septic arthritis can affect other bony sites
and joints (Fig. 5). This can arise as a complication of diabetic foot
infections (Fig. 6) or as a result of trauma or as a complication of
surgical intervention.
S aureus
pneumonia can develop after aspiration of oral secretions
or from the haematogenous spread of the organism from a distant
site. Empyema can develop as a complication of pneumonia.
Clinical features
Clinical features of
S aureus
infections in patients with diabetes are
essentially the same as in people without diabetes. Patients with IE
may present with non-specific influenza-like symptoms and weight
loss. Their condition can deteriorate rapidly and include disruption
of cardiac output and evidence of septic embolisation.
Osteomyelitis is usually characterised by localised pain over
the involved bone and fever.
S aureus
osteomyelitis that occurs
after trauma or a surgical procedure is generally accompanied by
inflammation and purulent discharge from the wound or the sinus
tract overlying the infected bone. The symptoms of spondylodiscitis
are usually non-specific back or neck pain. A third of cases can
develop neurological deficits, including leg weakness, paralysis,
sensory deficit, radiculopathy and sphincter loss.
37
This is more
likely when there are associated epidural abscesses, the diagnosis
is delayed or when there are cervical lesions.
34,38
Diabetes mellitus,
advanced age and steroid use are risk factors for paralysis.
34,39
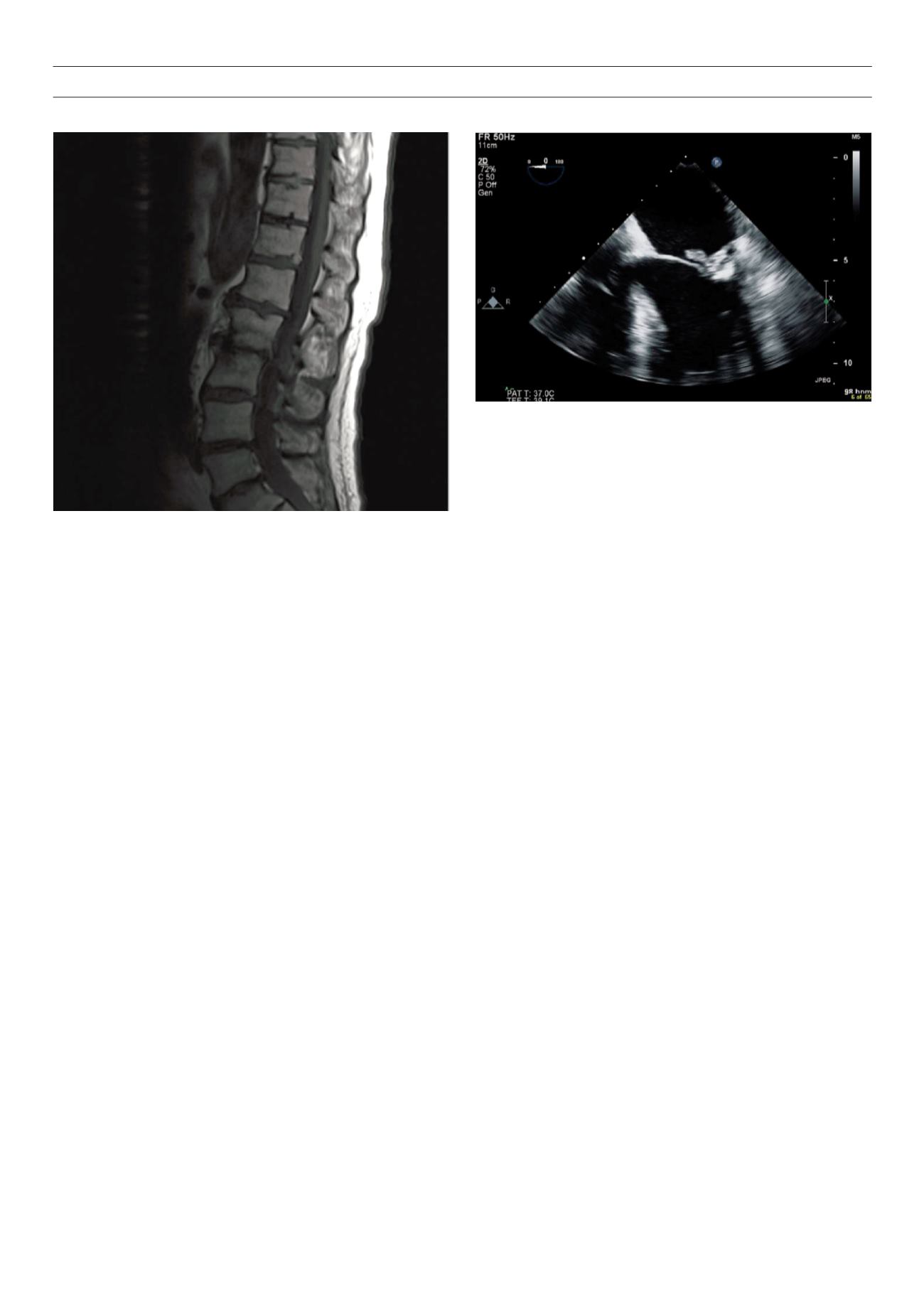
Figure 3.
Magnetic resonance image (MRI) of spine of a patient with type 2
diabetes and
S aureus
bacteraemia. The patient presented with non-specific
back pain and fever. MRI scan showed discovertebral osteomyelitis at T5/6 with
an associated right paraspinal abscess. He was treated with intravenous (IV)
flucloxacillin followed by daptomycin as out-patient parenteral antimicrobial
therapy to complete 8 weeks of IV therapy, followed by oral flucloxacillin to
complete 12 weeks.
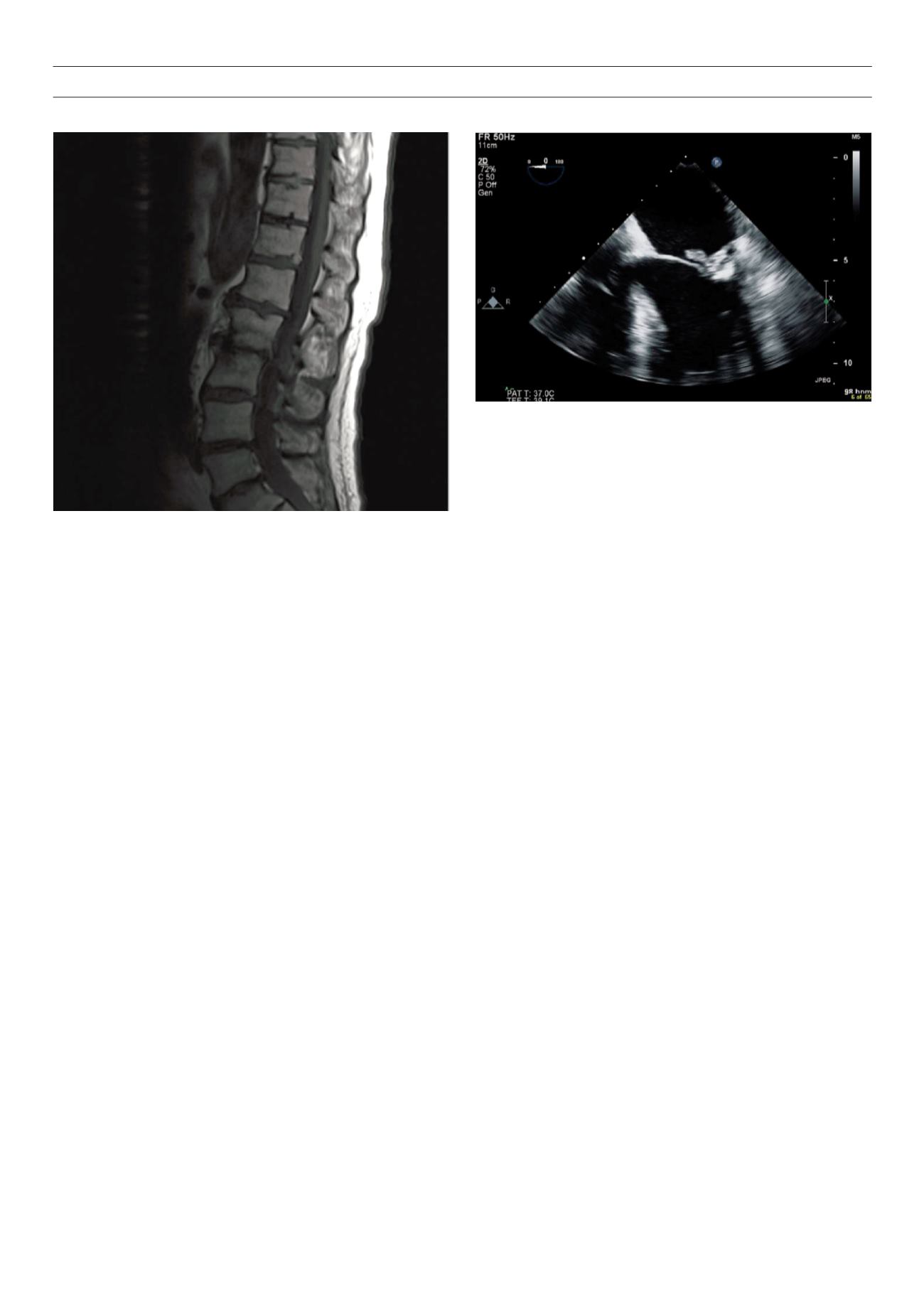
Figure 4.
Transoesophageal echocardiography (TOE) image of a patient with
S aureus
bacteraemia and type 2 diabetes. She had a past history of prosthetic
tissue aortic valve replacement. The patient initially presented with
S aureus
bacteraemia secondary to infection of paraspinal muscles. Initial TOE did not
show any vegetations. She received 4 weeks of intravenous IV and 4 weeks of
oral flucloxacillin and made good progress. However she presented 2 months
later with recurrence of
S aureus
bacteraemia. A repeat TOE shown here con-
firmed native valve infective endocarditis. The patient was managed conserva-
tively with IV daptomycin due to a rash with flucloxacillin.
Necrotisingpneumoniausuallypresentswithmassivehaemoptysis
and septic shock.
12
Clinical manifestations of staphylococcal toxic
shock syndrome start abruptly and include fever, hypotension, and
a diffuse, macular erythematous rash. Multiple organ systems are
also involved, and the entire skin, including the palms and soles,
desquamates. A particularly virulent form of toxic shock syndrome
is purpura fulminans. This disease is characterised by large purpuric
skin lesions, fever, hypotension and disseminated intravascular
coagulation.
7
Investigations
Microscopy and culture of specimens are vital in the confirmation of
S aureus
infection. The successful detection of organisms in a clinical
specimen depends on the type of the infection (abscess, bacteraemia
etc.) and the quality of the material submitted. A swab submitted
after scraping the base of an abscess should show an abundance of
organisms on Gram stain. Aspirated pus however consists primarily
of necrotic material with relatively few organisms.
7
It is important to sendmultiple blood cultures before commencing
antibiotic therapy. Three sets of optimally filled blood cultures taken
from peripheral sites, with at least six hours between them, is
recommended in patients with chronic or sub-acute presentation of
IE. If patients with suspected IE present with severe sepsis or septic
shock however two sets of blood cultures are recommended within
one hour before commencing antibiotics.
40
There is no evidence
to support the commonly held view that blood cultures should be
taken from different sites.
40
Repeat blood cultures are recommended 48–96 hours after
commencing antimicrobial therapy.
Biopsy samples may be of value for bone infections. For patients
with spondylodiscitis, biopsies (either open or percutaneous) are
often reserved for patients with negative blood cultures. The
value of a percutaneous biopsy as a safe and minimally invasive
intervention is well established. Although some experts recommend
a second percutaneous biopsy if the first is negative others would