REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
40
VOLUME 11 NUMBER 1 • MARCH 2014
such as rifampicin or clindamycin. Although bactericidal, there are
concerns that at concentrations just above the MIC (likely with
poor penetration into necrotic tissue) flucloxacillin may increase
PVL production as it does in vitro.
78
Intravenous immunoglobulin
(IVIG) should be considered in addition to intensive care support
and high-dose antimicrobial therapy because of its action in
neutralising exotoxins and superantigens, particularly enterotoxins
A, B and C and TSST-1. The dosage of 2 g/kg of IVIG recommended
for streptococcal toxic shock syndrome
12,79
may be applicable for
PVL
S aureus
infection, and may be repeated after 48 hours if there
is still evidence of sepsis, or failure to respond. It is very important
to undertake early surgical debridement.
12
Imaging modalities may help identify the source of
S aureus
bacteraemia and the extent of the infection with any metastatic
spread. Surgical input may be needed for source clearance.
Surgical management
S aureus
is the predominant pathogen in diabetic foot infections.
Clinicians should seek urgent surgical consultation for patients
presenting with evidence of a life- or limb-threatening infection,
necrotising fasciitis or if the involved limb has critical ischaemia.
80
Surgical input is also required for evidence of a deep-space
infection or abscess (Fig. 4). The most common site for a severe
foot infection is the plantar surface. A plantar wound accompanied
by dorsal erythema or fluctuance suggests that the infection has
passed through fascial compartments, likely to require surgical
drainage. Prompt and adequate surgical debridement, including
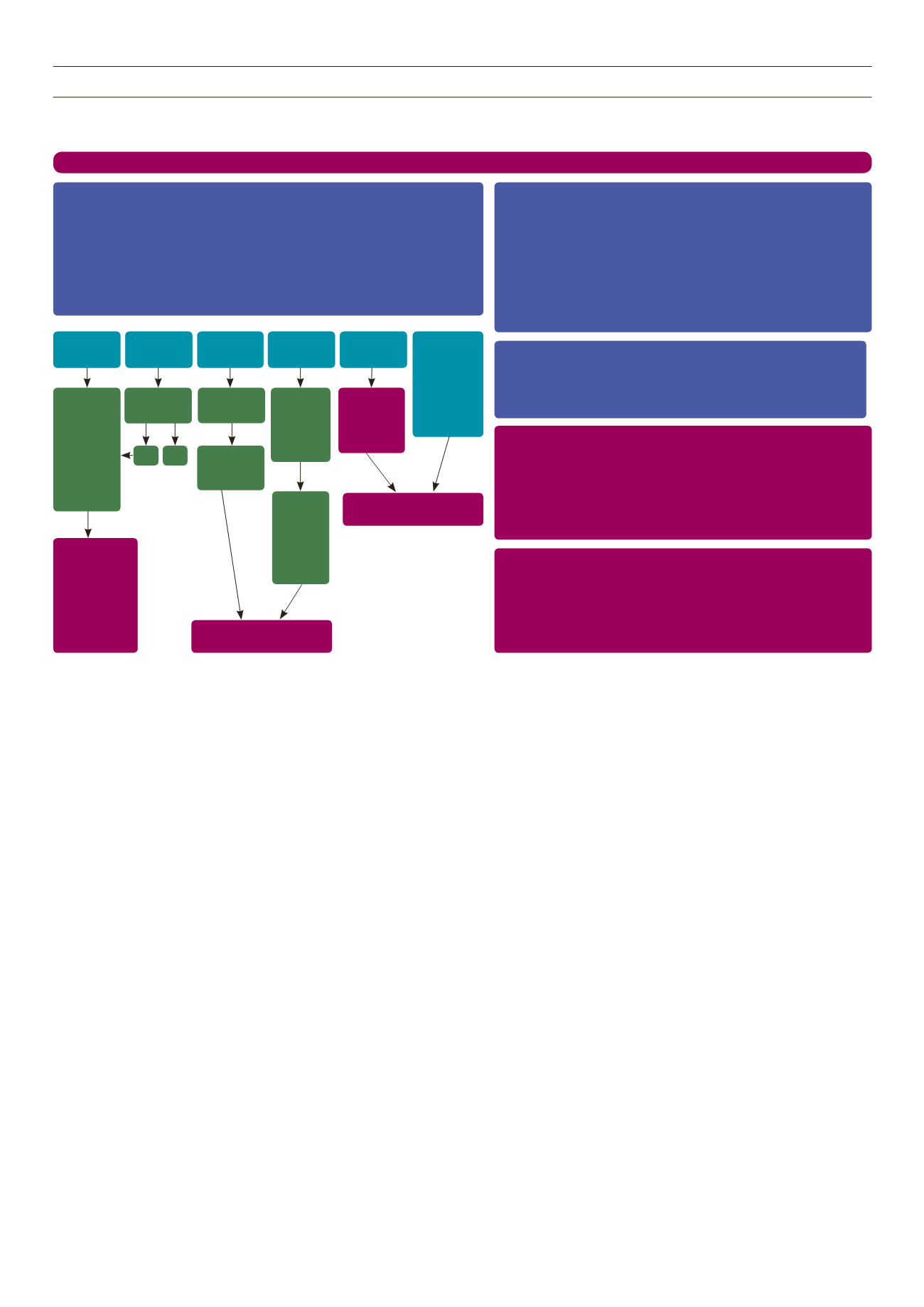
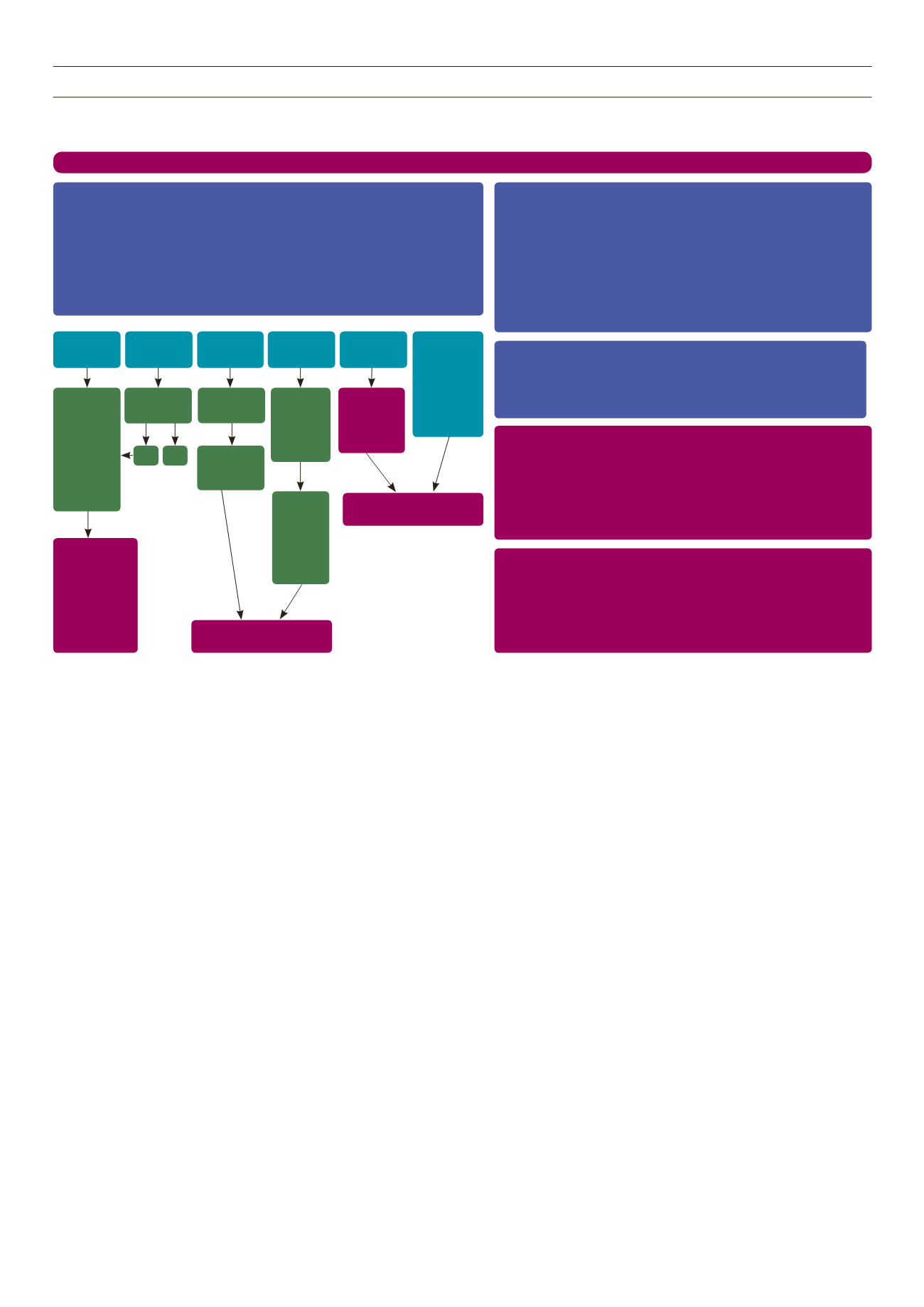
Figure 7.
Guidance on management of proven suspected
Staphylococcus aureus
bacteraemia in adults. Reproduced with the permission of the Scottish Antimicrobial
Prescribing Group.
88
limited resection or amputation, may decrease the likelihood that
a more extensive amputation is needed.
81, 82
Development of an
abscess within the foot, especially in the presence of ischaemia, can
rapidly lead to irreparable tissue damage. Prolonged duration of
antibiotic therapy is required for osteomyelitis. This may be in part
due to the observation in experimental models that
S aureus
can
persist following digestion by osteoblasts.
83
In addition, antibiotic
penetration intobonemay be unreliable in some patients, particularly
in those with vasculopathy as in patients with diabetes.
Cardiac surgery is indicated for patients with IE when they
develop uncontrolled heart failure, uncontrolled infection or when
they are at risk of embolic events. Patients with aortic or mitral
valve IE who develop severe acute regurgitation or valve obstruction
causing refractory pulmonary oedema, and patients who develop
a fistula into a cardiac chamber or pericardium causing refractory
pulmonary oedema should be considered for emergency cardiac
surgery. Patients with locally uncontrolled infection (including
abscess, false aneurysm, enlarging vegetation), persisting fever
and positive blood cultures for 10 or more days after commencing
appropriate antimicrobial therapy and infections caused by multi-
resistant organisms should also be considered for cardiac surgery.
Large aortic and mitral valve vegetations (> 10 mm) with one or
more embolic episodes despite antibiotic therapy and isolated
very large vegetations (> 15 mm) are also indications for cardiac
surgery.
40,47
The management of PJI almost always necessitates the need for
surgical intervention and prolonged courses of intravenous or oral
Guidance on management of proven or suspected
Staphylococcus aureus
bacteraemia in adults
Staphylococcus aureas
bacteraemia suspected or indentified in the laboratory. Consider rapid identification test if available.
Initial management – attending clinician
Check for signs of sepsis and assess severity. Initiate fluid resuscitation if required.
•
Ensure prompt administration of empirical antibiotic therapy following local policy.
•
Look for potential source of infection: skin (cellulitis, ulcer, site of current or recent indwelling medical service,
•
drug use by injection, surgical site infection), septic DVT, bone or joint inflammation (specifically paravertebral
tenderness), prosthesis, urinary catheter, endocarditis (ausculate heart, examine for heart murmur or stroke in
the context of sepsis and cutaneous stigmata of endocarditis), pneumonia (chest Xray).
Consider recent medical history – hospitalisation, vascular device, drug use by injection or previous SAB.
•
Consider need for further microbiology samples if evidence of infection e.g. swab from ulcer or IV device site,
•
MSSU/CSU, sputum sample
Discuss with senior clinician in all cases.
•
Repeat blood cultures (BC in 48–76 hours and if ongoing fever despite antibiotic therapy
•
Initial management – attending clinician
Check for signs of sepsis and assess severity. Initiate fluid resuscitation if required.
•
Ensure prompt administration of empirical antibiotic therapy following local policy.
•
Look for potential source of infection: skin (cellulitis, ulcer, site of current or recent indwelling
•
medical service, drug use by injection, surgical site infection), septic DVT, bone or joint
inflammation (specifically paravertebral tenderness), prosthesis, urinary catheter, endocarditis
(ausculate heart, examine for heart murmur or stroke in the context of sepsis and cutaneous
stigmata of endocarditis), pneumonia (chest Xray).
Consider recent medical history – hospitalisation, vascular device, drug use by injection or previous
•
SAB.
Consider need for further microbiology samples if evidence of infection e.g. swab from ulcer or IV
•
device site, MSSU/CSU, sputum sample
Discuss with senior clinician in all cases.
•
Repeat blood cultures (BC in 48–76 hours and if ongoing fever despite antibiotic therapy
•
ECHOCARDIOGRAPHY
Discuss the need for a transthoracic echocardiogram (TTE) with a cardiologist for all patients with
•
SAB while the patient is receiving IV anti-staphylococcal therapy.
Consider transoesophageal echocardiogram (TDE) in patients at high risk of endocarditis:
•
persistent bacteraemia > 4 days, permanent intra-cardiac device, TTE negative AND repeat BC
Positive, source unknown.
EMPIRICAL ANTIBIOTIC THERAPY
Assess clinical risk to determine likelihood of MRSA considering previous MRSA, admission
•
from residential care, wound or indwelling vascular device, community or healthcare acquired
infection.
Risk assessment negative, treat as MSSA – IV flucloxacillin 2g 4–6 hourly (assuming normal renal
•
function).
Risk assessment positive, treat as MRSA – local vancomycin protocol.
•
Penicillin allergy – use vancomycin first line for MSSA and MRSA.
•
In patients with intolerance, vancomycin allergy treatment failure or if clinical concern regarding
•
response discuss alternative therapy with ID physician or clinical microbiologist.
VANCOMYCIN THERAPY
Intermittent (pulsed) infusions: Aim for trough of 15-20 mg/l and consider increasing the dose /
•
dose frequency to achieve this level.
Continuous infusion: Aim for steady state concentration of 20-25 mg/l.
•
In patients or concomitant nephrotoxic drugs or with impaired renal function monitor levels
•
closely and seek specialist advice on tailoring dosage.
If poor clinical response to vancomycin MIC testing by E-test recommended. If MIC > 1.0 mg/1
•
by E-test and patient not reponding switch to alternative antibiotic and continue search for
underlying focus.
Septic
arthritis or
Osteomyetitis
SS7l /SSI /
infected
Ulcer
Indwelling IV
device
Source
unknown
Infective
endocarditis
Other potential
primary sources
include
• Pneumonia
• Urinary tract
• Haemodialysis
– related
• Drug use by
injection
Treat as per
local / British
Society for
Antimicroxial
Chemotherapy
guidelines
TTE
negative,
repeat BC
negative
and no
ongoing
symptoms
Remove device
if possible
Repeat BC
negative and
no ongoing
symptoms
Poor response
to treatment
Yes
No
Considerand
discuss:
•Orthopaedic
review
• Imaging
–MRA /CT
/nuclear
medicine
• Intervention
–aspiration
/washcut
/device removal
Minimum2weeks:
IV therapyoras
advisedby ID
physicianorclinical
microbiologist
Septicarthritis:
further2weeks IV
/oralorasadvised.
Osteomycitis:at least
4 furtherweeks IV /
oralorasadvised.
Discuss treatmentwith IDphysicianor
clinicalmicrobiologist
Discuss treatmentwith IDphysicianor
clinicalmicrobiologist
Noongoing
concern
regarding
cardiac,
bone, joint,
prostheticor
otherdeep
source