
VOLUME 11 NUMBER 4 • NOVEMBER 2014
147
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
intuitive, however, it must be noted that the kidney may be reacting
to perceived inadequate intracellular glucose levels.
Mechanism of action of SGLT inhibitors
Inhibition of SGLT limits re-absorption of glucose fromthe glomerular
ultra-filtrate in the proximal convoluted tube. This increases urinary
glucose excretion.
Increased urinary glucose excretion directly ameleriorates hyper-
glycaemia. In addition, reduction in blood glucose levels results in
the reduction of glucotoxicity and consequently improves beta-
cell function and insulin resistance.
16
This mode of action targets
(directly and indirectly) three pathological hallmarks of type 2
diabetes mellitus, hyperglycaemia (directly), beta-cell dysfunction
(indirectly), and insulin resistance (indirectly). Fig. 1 shows the site
of action of SGLT inhibitors.
Effects extrapolated from the mechanism of action
This section extrapolates possible effects from mode of action; it
is based on intuition and not clinical data. The section that follows
this attempts to link potential effects to data from clinical studies.
Given that the kidney is removing increased amounts of glucose,
one may expect the class to ameliorate hyperglycaemia and have
a potential to increase hypoglycaemic episodes. Increased urinary
glucose excretion may reduce available calories and consequently
could result in weight loss.
Osmotic diuresis may lower blood pressure. However, osmotic
diuresis has the potential to result in volume depletion. Osmotic
diuresis may also increase the frequency of urinary voiding.
Due to the inhibition of renal SGLT, increased urinary glucose
excretion may serve as a substrate for micro-organisms and thus
potentially increase the risk of urinary tract and genital infections. In
addition, high urinary glucose concentrations may adversely impact on
the cells lining the urinary tract and thus impair the innate immunity of
the urinary tract and predispose to urinary tract infections.
Lowering blood glucose levels, the glucotoxic effect of glucose
is diminished irrespective of the degree of beta-cell function. This
potentially protective mechanism of action on the beta-cells could
result in more residual beta-cells and hence insulin production
being maintained. This beta-cell-independent mode of action will
mean that the class is potentially efficacious despite the severity of
beta-cell depletion/dysfunction.
The ability of this class to work independently of beta-cell
dysfunction and insulin resistance allows a potentially synergistic
action with other anti-diabetic drugs. It may also allow lower doses
of anti-diabetic agents to be used, which may reduce the risk of
adverse effects.
Table 3 lists potential theoretical advantages and disadvantages
of the effects extrapolated from the mode of action.
Clinical experience with SGLT inhibitors
This section attempts to compare theoretical effects expected
from the mode of action of the SGLT inhibitors with actual clinical
findings.
Table 3.
Potential advantages and disadvantages extrapolated from
mode of action
Potential advantages
Potential disadvantages
Efficacy not limited by degree of
beta-cell impairment or insulin
resistance
Increased urinary frequency
Weight loss
Volume depletion
Blood pressure reduction
Hypoglycaemia
Reduces glucose toxicity and
indirectly improves insulin resistance
and beta-cell dysfunction
Increased urinary tract and genital
infections
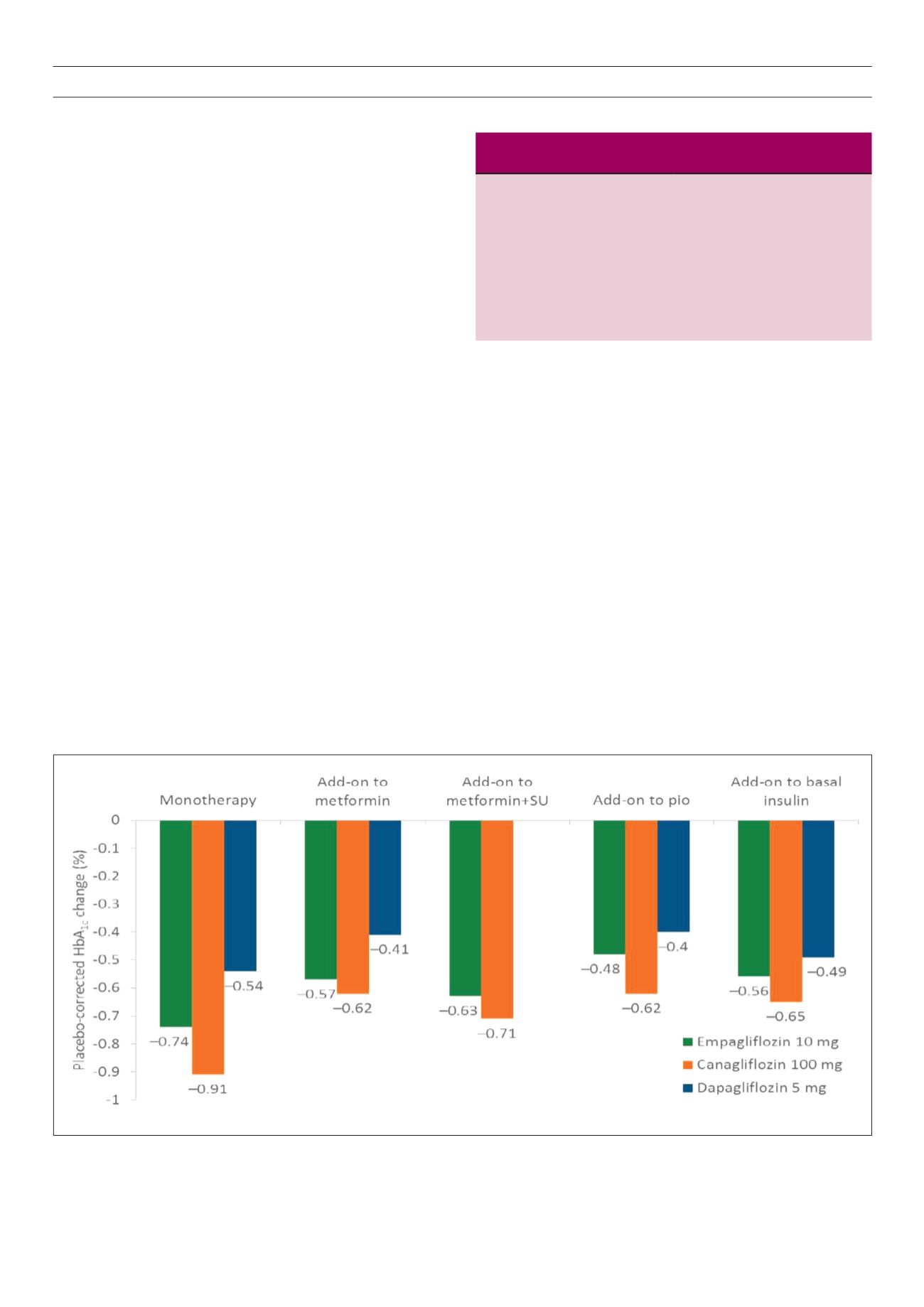
Fig. 2.
Placebo corrected HbA
1c
for SGLT2 inhibitors in different subgroups of patients.
19-25



















