
152
VOLUME 11 NUMBER 4 • NOVEMBER 2014
REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
one-fifth for cardiology, contributing to around 20% of their total
costs. Extrapolating these data to the UK as a whole, they estimated
that £1.00 in every £8.00 spent on hospital care in the UK was
spent on a patient with diabetes.
25
Hospital costs incurred in the
final years of life have also been shown to be greater in patients
with diabetes than those without diabetes at a ratio of 1.39 (
p
<
0.001) after standardisation for age and gender, and accounted for
15.6% of revenue.
26
It is not just the direct cost to healthcare services that is important,
the non-health-service costs (including the social and productivity
costs of diabetes) are considerably higher and are largely borne
by the individual or their carers. Diabetes was estimated to cost
approximately £23.7 billion in the UK in 2010/2011, with non-
health-service costs accounting for £13.9 billion of this figure. If
no changes are made to the way diabetes is treated by 2035/2036
then costs are expected to increase further, with direct healthcare
costs representing around 17% of NHS expenditure at £16.9 billion
and non-health-service costs increasing to £22.9 billion.
23
Additional
studies investigating the incidence and prevalence of diabetes from
2000 to 2060 estimate that a 3% annual increase in the UK resident
population is likely to disguise a much greater increase among the
elderly, resulting in a 20% increase in the number of people with
type 2 diabetes from 2000 to 2030 and inflicting an increasingly
large burden on the UK health service.
27
Cardiovascular risk factors in patients with diabetes
The INTERHEART study arguably provides the most comprehensive
global picture of the relative contribution of major modifiable risk
factors to CVD.
28
INTERHEART is a case–control study of acute
myocardial infarction (MI) which enrolled almost 30 000 individuals
from 52 countries, representing every inhabited continent. The study
investigated the relationship of CVD risk factors such as smoking,
hypertension, diabetes, blood lipids, diet and exercise to MI. It was
found that smoking, a raised apolipoprotein B: apolipoprotein A1
(ApoB:ApoA1) ratio, history of hypertension, diabetes, abdominal
obesity, and psychosocial factors were all associated with a significant
increase in the risk of acute MI. Daily consumption of fruit and
vegetables, regular alcohol consumption and regular physical activity
were all associated with a significant decrease in the risk of acute
MI (
p
< 0.0001 for each risk factor other than
p
= 0.03 for alcohol).
These associations were noted in men and women, across all age
ranges and in all regions of the world. Collectively, these nine risk
factors accounted for 90% of the population-attributable risk (PAR)
for MI in men, and 94% in women.
28
Some of the increased cardiovascular risk in patients with diabetes
can be explained by a clustering of traditional risk factors within
this population, and it has long been established that people with
diabetes are more likely to have additional cardiovascular risk factors
than those without diabetes.
29,30
Data from the UKPDS show that
in patients with type 2 diabetes, increased concentrations of low-
density lipoprotein (LDL), decreased concentrations of high-density
lipoprotein (HDL), hyperglycaemia, hypertension and smoking are
risk factors for coronary artery disease,
31
with all factors other than
increased LDL also risk factors for peripheral vascular disease.
32
The
MRFIT study also found that, compared with men without diabetes,
12-year CVD mortality rates were much higher at every level of
serum cholesterol, systolic blood pressure and smoking among
diabetic men.
30
In addition, a number of randomised trials that
investigated the effect of intensified intervention on a single risk
factor in patients with type 2 diabetes demonstrated microvascular
benefits in the eyes and nerves and both micro and macrovascular
benefits in the kidneys.
17,33,34,35
For this reason, both national and international guidelines for the
management of type 2 diabetes advocate a multifactorial approach
including the treatment of risk factors such as hypertension,
dyslipidaemia and encouraging smoking cessation in addition to
glycaemic control.
36,37,38
The effect of implementing a multifactorial
treatment approach for cardiovascular risk in patients with diabetes
was evaluated in the STENO-2 study. This relatively small study
of 160 patients compared an intensive, targeted, multifactorial
intervention (including both behavioural and pharmacological
therapy) to conventional treatment, and found that patients
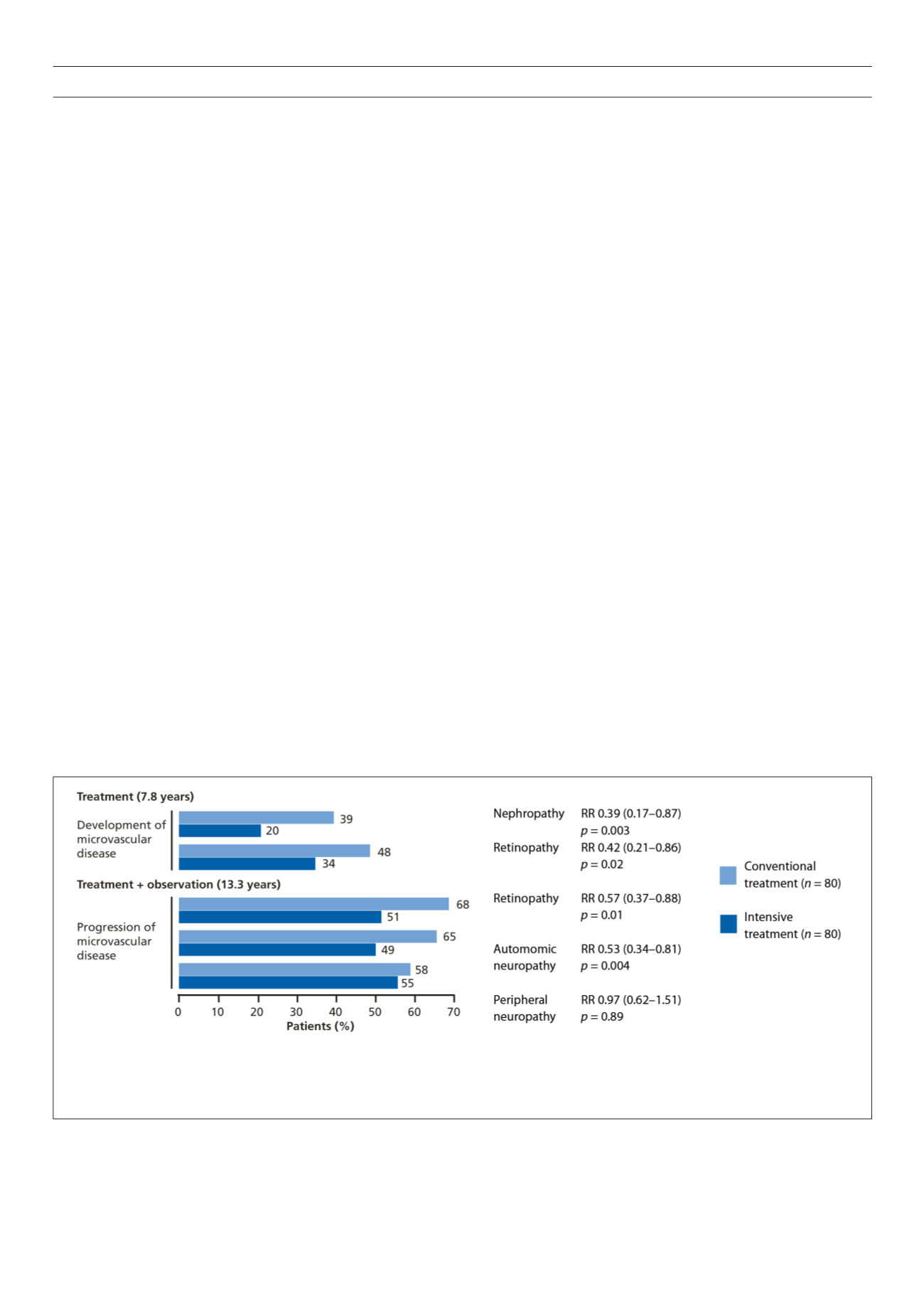
RR, relative risk (95% CI)
Diabetic nephropathy was defined as urinary albumin excretion > 300 mg per 24 hours in two of three sterile urine specimens. Diabetic retinopathy was graded according to the six-level grading scale of
the European Community-funded Concerted Action Programme into the Epidemiology and Prevention of Diabetes by two independent ophthalmologists who were unaware of treatment assignment.
Peripheral neuropathy was measured with a biothesiometer. Autonomic neuropathy was diagnosed based on measurement of the RR interval on an ECG during paced breathing and an orthostatic
hypotension test conducted by a laboratory technician who was unaware of patients’ treatment assignment
Figure 1.
Intensive multifactorial intervention in the STENO-2 study significantly reduced the development or progression of diabetes-related microvascular disease,
but failed to prevent this in many patients.
39,40,67



















