
VOLUME 11 NUMBER 4 • NOVEMBER 2014
153
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
receiving intensive therapy had a significantly lower risk of CVD (HR
0.47, 95% CI 0.24–0.73), nephropathy (HR 0.39, 95% CI 0.17–
0.87), retinopathy (HR 0.42, 95% CI 0.21–0.86) and autonomic
neuropathy (HR 0.37, 95% CI 0.18–0.79).
39
The mortality benefits
of such an intervention were also investigated in an extension
of the STENO-2 study (mean 13.3 years follow-up), where the
multifactorial intervention was shown to have a sustained benefit
on both vascular complications and cardiovascular mortality.
40
Y
et
al
though a comprehensive risk factor approach is essential when
treating patients with type 2 diabetes, data from the STENO-2
study show that despite reductions versus conventional treatment,
multifactorial interventionis insufficient to prevent the development
or progression of microvascular disease in up to 50% of patients
(Fig. 1). It is, therefore, clear that there is a need for renewed focus
on eff ective interventions that are capable of reducing the residual
risk of cardiovascular events and microvascular complications in
patients with type 2 diabetes receiving optimal therapy according
to current standards of care.
Quantifying cardiovascular risk
Patients with type 2 diabetes benefit from sustained and early
intervention for risk factor control; however, treatment interventions
are often initiated too late for maximum CVD benefit. Ensuring that
we are quantifying risk correctly is crucial to achieving early risk
factor control and addressing the residual cardiovascular risk seen
in type 2 diabetes patients.
The concept of medical intervention based on estimated total
CVD risk in asymptomatic patients is well established both in the
UK
41
and internationally.
42,43
Underpinning this are studies such as
the Framingham Heart Study, which to date has enrolled three
generations of participants to identify the common factors or
characteristics that contribute to CVD.
44
These data have enabled
researchers to construct multivariate risk prediction algorithms
intended to provide an estimate of CHD or CVD risk over a specified
time period, generally 10 years.
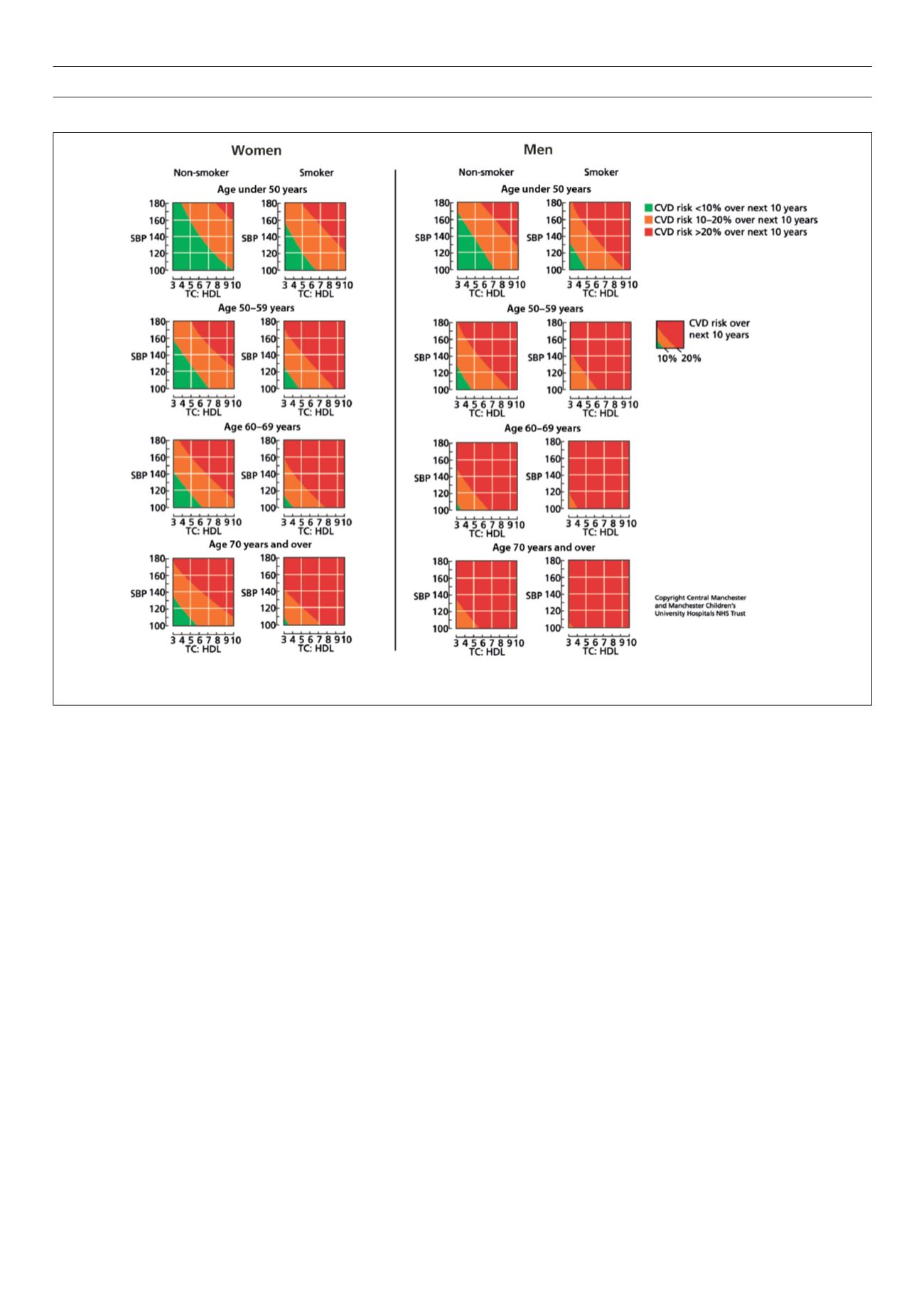
The second edition of the Joint British Societies’ guidelines on
cardiovascular disease in clinical practice (JBS-2) uses a risk estimate
tool adapted from the equations published from the Framingham
study in 1991.
45
The tool estimates total CVD risk (a combined
endpoint of CHD, stroke and transient cerebral ischaemia) for an
asymptomatic individual from several, wellestablished risk factors
such as age, sex, smoking habit, systolic blood pressure and ratio of
total cholesterol to HDL cholesterol.
This is then expressed as a probability of developing CVD over 10
years, based on the number of cardiovascular events expected over
10 years in 100 men or women with the same risk factors as the
individual being assessed. Charts have subsequently been created
to easily assess risk based on these factors (Fig. 2), and are split into
Reproduced from British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, Stroke Association. Joint BritishSocieties' guidelines on prevention of
cardiovascular disease in clinical practice.
Heart
2005;
91
(suppl 5). With permission from BMJ Publishing Group
Figure 2.
JBS2 CVD risk prediction charts for men and women.
41



















