
154
VOLUME 11 NUMBER 4 • NOVEMBER 2014
REVIEW
SA JOURNAL OF DIABETES & VASCULAR DISEASE
CVD risk categories of ≥ 10%, ≥ 20% and ≥ 30% over 10 years.
Asymptomatic individuals with a CVD risk of ≥ 20% are classified
as high risk, with this level being a threshold for treatment with
antihypertensive and lipid-lowering therapies. It should be noted that
charts have not been created for patients with diabetes, and several
studies have suggested that these types of equations considerably
underestimate the risk of both cardiovascular disease and mortality
in this group.
46-48
Guidelines instead recommend all patients with
diabetes should be considered high risk and managed to the same
lifestyle and defined risk-factor targets as individuals with established
CVD and others at high 10-year risk of developing CVD.
41
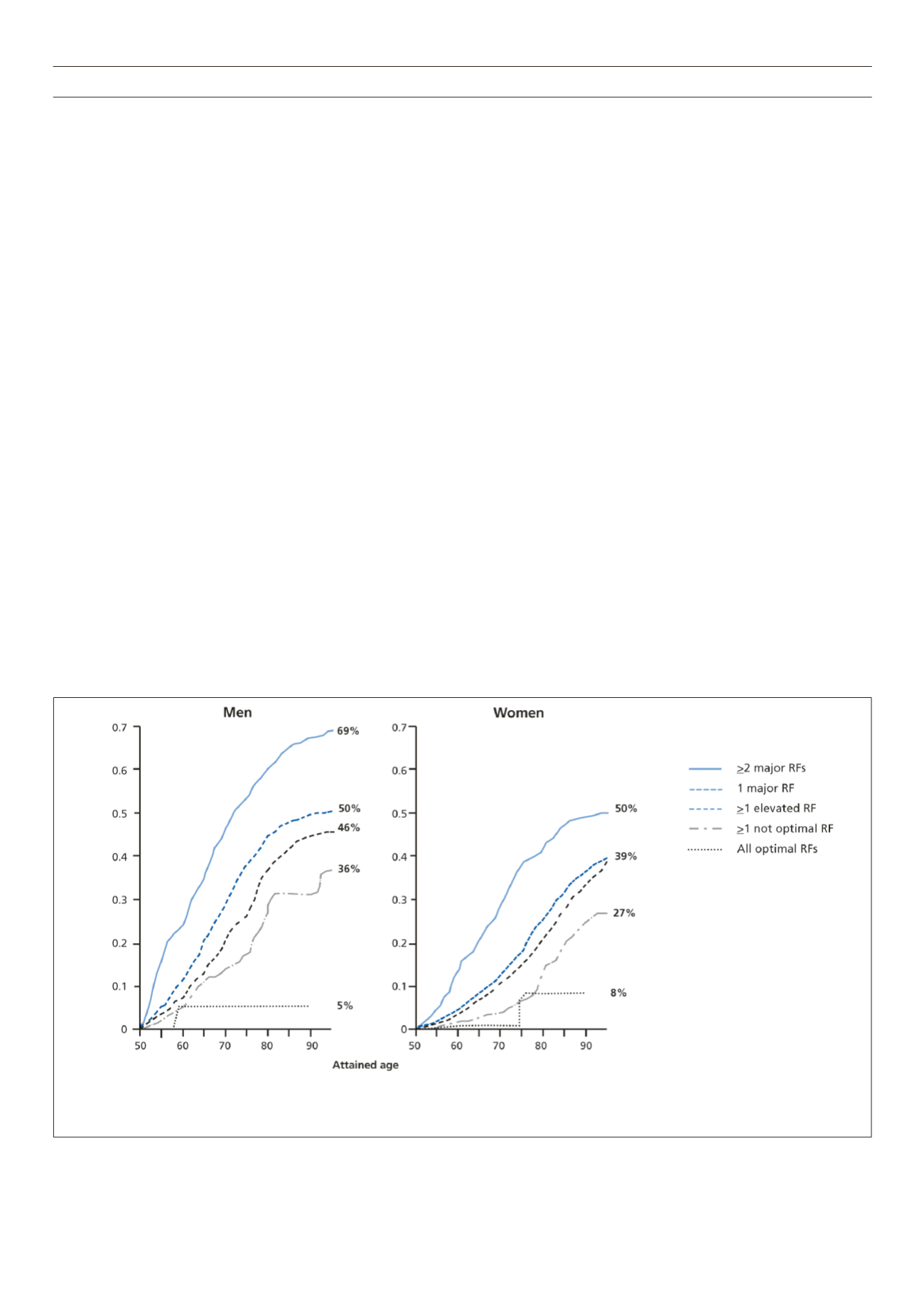
However, there are well recognised limitations to a 10-year risk
metric for the calculation of cardiovascular risk. The 10-year risk
metric is dominated by two particular risk factors – chronological
age and gender. This fact effectively disenfranchises the middle-
aged and females, resulting in a delay in initiating treatment until a
particular chronological age is reached. Lloyd-Jones and colleagues
evaluated data from the Framingham Study to examine the lifetime
burden of CVD by traditional risk factor burden at 50 years of age.
Participants were stratified into five mutually exclusive categories,
as shown in Fig. 3, and they found that an absence of risk factors
at 50 years of age is associated with a very low lifetime risk for CVD
(5.2% for men and 8.2% for women). Conversely, those with two
or more major risk factors for CVD at 50 years of age had a markedly
higher lifetime risk (68.9% for men and 50.2% for women), and
for both men and women the adjusted cumulative incidence curves
across risk strata separated early from those without risk factors
and continued to diverge throughout the lifespan.
49
The importance of early risk-factor intervention is reinforced
by observational data from patients with a nonsense mutation in
the gene PCSK9 (proprotein convertase subtilisin/kexin type 9),
resulting in lifelong reductions in LDL cholesterol. It was found
that in those with the mutation, a 28% lifetime reduction in mean
LDL cholesterol translated into an 88% reduction in the risk of
CHD (
p
= 0.08 for the reduction; HR: 0.11, 95% CI: 0.02–0.81).
50
Moreover, a recent meta-analysis of published data has estimated
the effect of long-term exposure to lower LDL cholesterol on the
risk of CHD mediated by nine poly-morphisms in six different genes.
Mendelian randomisation studies were combined in this meta-
analysis and showed that all nine polymorphisms were associated
with a highly consistent reduction in the risk of CHD per unit
lower LDL cholesterol with no evidence of heterogeneity of effect.
A meta-analysis combining non-overlapping data from 312 321
participants revealed that naturally random allocation to long-term
exposure to lower LDL cholesterol was associated with a 54.5%
reduction in the risk of CHD for each mmol lower LDL cholesterol.
This represents a three-fold greater reduction in the risk of CHD
per unit lower LDL cholesterol than that observed during treatment
with a statin started later in life.
51
It is clear, therefore, that the use of a 10-year risk metric
disenfranchises clinicians to control risk factors in younger patients
and treatment interventions are often initiated too late for maximum
CVD benefit. For this reason, the third edition of the Joint British
Societies guidelines (JBS3) is expected to advocate a move from
the current 10-year risk score to a lifetime CVD risk calculator. The
lifetime risk calculator will tell patients how likely they are to suffer
a cardiovascular event at various points in their lives.
It is likely that this move to assessing lifetime risk will result in
intervention to reduce cardiovascular risk at an earlier stage.
When should we intervene to reduce cardiovascular
risk?
In recent years, it has become increasingly clear that despite the
impressive gains made through the use of 10-year risk calculators,
Optimal risk factors are defined as total cholesterol < 4.65 mmol/l (< 180 mg/dl), blood pressure < 120/< 80 mmHg, non-smoker, and non-diabetic. Not optimal risk factors are defined as total cholesterol
of 4.65 to 5.15 mmol/l (180 to 199 mg/dl), systolic blood pressure of 120 to 139 mmHg, diastolic blood pressure of 80 to 89 mmHg, non-smoker, and non-diabetic. Elevated risk factors are defined as
total cholesterol of 5.16 to 6.19 mmol/l (200 to 239 mg/dl), systolic blood pressure of 140 to 159 mmHg, diastolic blood pressure of 90 to 99 mmHg, non-smoker, and non-diabetic. Major risk factors
are defined as total cholesterol ≥ 6.20 mmol/l (≥ 240 mg/dl), systolic blood pressure > 160 mmHg, diastolic blood pressure > 100 mmHg, smoker, and diabetic.
Figure 3.
Remaining lifetime risk for cardiovascular disease in men and women at 50 years of age
49



















