30
VOLUME 17 NUMBER 1 • JULY 2020
CASE REPORT
SA JOURNAL OF DIABETES & VASCULAR DISEASE
[glucose level 1 091 mg/dl (60.55 mmol/l)] and diabetic ketoacidosis
(serum bicarbonate level 6.8 mmol/l). Additionally, leukocytosis
(white blood cell count 20.90 × 103 cells/μl) and hyperkalaemia (K
+
5.3 mmol/l) were noted.
Under suspicion of diabetic ketoacidosis, an insulin pump (insulin
actrapid 50 units usage in 500 ml normal saline) was immediately
administered at a rate of 60 ml/h. However, cardiac arrest occurred
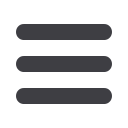
abruptly. An electrocardiogram revealed pulseless VT (Fig. 1) and
CPR was immediately performed with sequential defibrillation,
which was repeated five times. Laboratory data revealed severe
hypokalaemia (K
+
1.6 mmol/l). Large-dose inotropes including
dopamine (17.3 mcg/kg/min) and norepinephrine (26.5 mcg/kg/
min) were administered. Simultaneously, continuous KCl infusion
was performed. However, the haemodynamic status remained
inadequate with refractory VT and low cardiac output.
Peripheral VA-ECMO implantation was therefore performed
through the right femoral vein and artery at a pump speed of
3 000 rpm and flow rate of 3.3 l/min. A Glasgow coma scale
result of E2M2Vt was observed. Blood pressure was approximately
70/60 mmHg irrespective of the high doses of inotropes, and
occasional VT was noted despite anti-arrhythmia medication.
Moreover, echocardiography revealed generalised hypokinesia
of the bilateral ventricles with left ventricular ejection fraction of
10–15%. However, despite the VA-ECMO support, the patient
developed multiple organ dysfunction, including acute kidney
injury, congestive liver and severe pulmonary oedema.
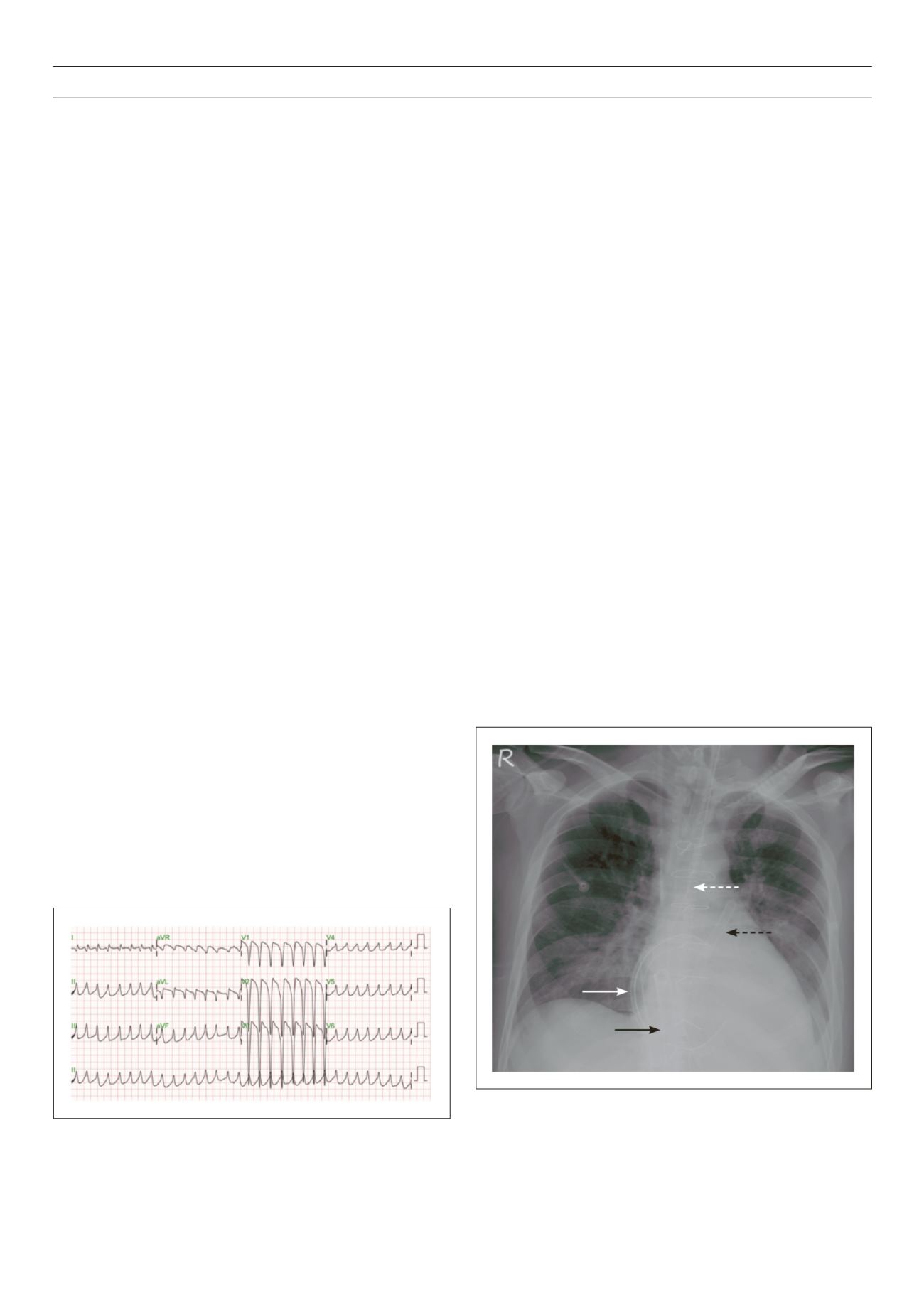
We therefore changed the VA-ECMO to a temporary
continuous-flow Bi-VAD (Levitronix
®
CentriMag) for better systemic
perfusion (Fig. 2). Using a sternotomy and under the guidance
of transoesophageal echocardiography, the left ventricular assist
device (L-VAD) inflow tube was inserted from the right superior
pulmonary vein into the left ventricular apex, whereas the outflow
tube was cannulated on the ascending aorta.
The right VAD (R-VAD) inflow tube was inserted into the right
atrium, and the outflow tube was inserted into the pulmonary
artery. The operation time was approximately two hours. The
initial L-VAD pump speed was 3 700 rpm and flow rate was
4.74 l/min. The R-VAD pump speed was 3 000 rpm and flow rate
was 4.87 l/min (Table 1).
For severe hypoxaemia resulting from pulmonary oedema,
an oxygenator was inserted into the L-VAD outflow to optimise
systemic oxygenation. Mean arterial pressure (MAP) was maintained
at 75–80 mmHg with low-dose norepinephrine (4.3 mcg/kg/min).
Potassium level was maintained within the range 4.2–4.7 mmol/l
and serum glucose level within 180–220 mg/dl (9.99–12.21 mmol/l).
At the time of maintaining support with Bi-VAD, the ventilator
was set at 40%
FiO
2
with positive end-expiratory pressure at
8 cmH
2
O to prevent alveolar collapse. The support pressure was
set at 12–15 cmH
2
O to achieve an optimal tidal volume status
(6–8 ml/kg), and the plateau pressure was controlled under
24 cmH
2
O. During the time of support with VAD, the patient’s MAP
was closely monitored and both VAD and inotropic agents were
gradually tapered down to prevent vasoconstriction in the vital
visceral organs.
Systemic heparinisation was performed to maintain an active
clotting time of 140–160 seconds to prevent thromboembolism.
Additionally, a broad-spectrum antibiotic was prophylactically
prescribed following the Bi-VAD implantation. On day three of
Bi-VAD implantation, the pulmonary oedema was completely
resolved; subsequently, the oxygenator was taken down from
the L-VAD outflow. Although renal function did not recover
immediately, it recovered completely after hospitalisation with
temporary haemodialysis (post-VAD implantation days one to
nine). Following 12-day support with the Bi-VAD, the myocardial
stunning was adequately improved; eventually, the Bi-VAD was
removed successfully.
Table 1 presents the biochemistry data, inotrope dosages and
echocardiography presentation during the VAD course. The patient
was weaned off the ventilator, and extubation was performed
three days after VAD removal. The day after extubation, the patient
was transferred to an ordinary ward and discharged one week later.
Out-patient follow up revealed normal cardiac and renal function
and cognition, and adequate control of diabetes.
Discussion
Hypokalaemia is a common electrolyte imbalance present in 20% of
hospitalised patients,
5
and some of these patients require immediate
Fig. 1.
Electrocardiogram demonstrating refractory ventricular tachycardia
despite correction for profound hypokalaemia.
Fig. 2.
The chest plain film demonstrates the L-VAD inflow tube from the right
superior pulmonary vein (solid white arrow), outflow tube into the ascending
aorta (dotted white arrow), R-VAD inflow tube from the right atrium (solid
black arrow), and outflow tube into the pulmonary artery (dotted black arrow).



















