VOLUME 17 NUMBER 1 • JULY 2020
33
SA JOURNAL OF DIABETES & VASCULAR DISEASE
CASE REPORT
Diabetes and thromboembolic risk
PETER ROSSING, MANESH PATEL
Correspondence to: deNovo Medica
website:
www.denovomedica.come-mail:
info@denovomedica.comPeter Rossing
Diabetologist, Copenhagen, Denmark
Manesh Patel
Cardiologist, Duke University, North Carolina, USA
Previously published by deNovo Medica, May 2020
S Afr J Diabetes Vasc Dis
2020;
17
: 33–37
Introduction
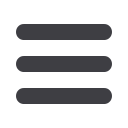
Today most practising clinicians are aware of the rampant spread
of diabetes throughout the world. Most estimates suggest that
diabetes affects between 30% and 35% of the population. This
report considers the interface between diabetes and cardiovascular
disease, which manifests as coronary artery disease, stroke and/
or peripheral arterial disease, chronic kidney disease (CKD), atrial
fibrillation (AF) and their individual and combined impacts on
prognosis. Professor Peter Rossing discusses the links between
diabetes and kidney disease and Professor Manesh Patel considers
the interrelationships between diabetes, AF, chronic kidney injury
and peripheral arterial disease, pointing out recent observations on
the effect of NOACs in these settings. A significant percentage of
patients with diabetes also have CKD; 28% will have albuminuria,
20% will have impaired renal function and 10% will have the
combination of both of these. Approximately 60% of diabetics have
normal kidney function (Fig. 1). Glycaemic control is important,
as glycaemia is related not only to the occurrence of micro- and
macrovascular complications in the kidneys, but also in the eyes,
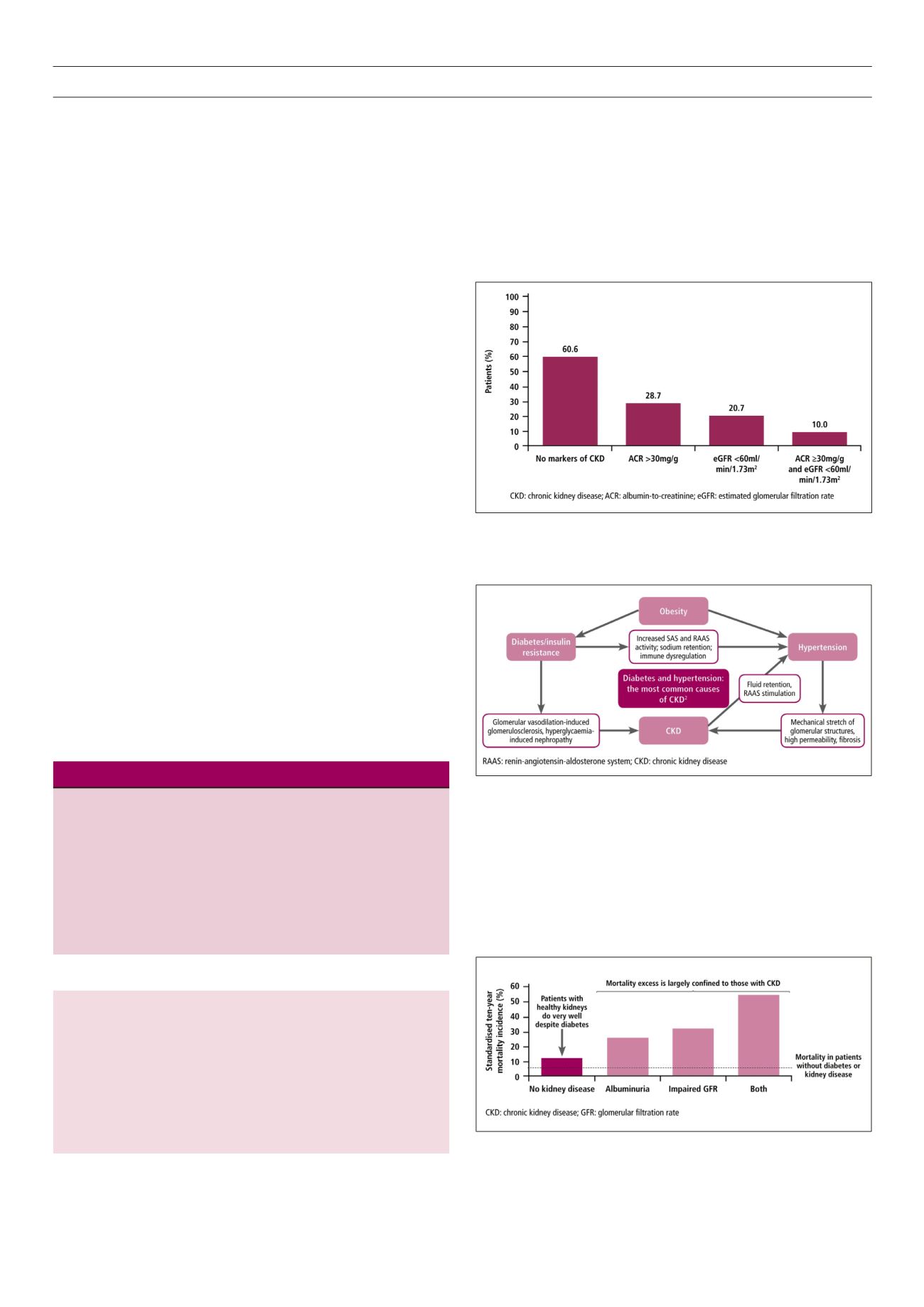
vascular system and heart. Type 2 diabetes mellitus (T2DM), often
associated with obesity, can lead to kidney disease either via the
metabolic pathway of hyperglycaemia or through a dynamic
pathway caused by hypertension that leads to intense pressure in
the kidney, glomerulosclerosis, fibrosis and the further increase of
blood pressure. Resultant progressive kidney disease can lead to
end-stage kidney disease (Fig. 2).
1-3
The impact of kidney disease affects the prognosis of the diabetic
patient. The risk of mortality is relatively low when there is no
kidney disease, but the presence of either albuminuria or impaired
renal function significantly increases that risk. A combination of
both proteinuria and impaired renal function significantly increases
10-year mortality in diabetes patients (Fig. 3).
4
Report and case study
Learning objectives
You will learn:
• The patient with diabetes is at increased risk of progressive kidney disease
• Diabetes increases the risk of developing atrial fibrillation; comorbidity is
associated with increased risk of death and cerebrovascular events
• Diabetic patients with atrial fibrillation show a trend toward slower
progression of acute kidney injury and reduced risk for end-stage renal
disease when using non-vitamin K antagonist oral anticoagulant therapy
in randomised controlled trials and real-world practice
• Diabetes patients with renal impairment have increased cardiovascular risk;
randomised controlled trial and real-world data show benefit of rivaroxaban
Fig. 1.
Kidney disease in diabetes patients – distribution of markers for CKD in
NHANES participants with diabetes, 2011–2014.
Fig. 2.
Diabetes increases the risk of kidney disease.
1-3
Fig. 3.
Mortality risk – impact of kidney disease in T2DM.
4



















