VOLUME 10 NUMBER 1 • MARCH 2013
23
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
Correspondence to: Dr Hilton Kaplan
Claremont, Cape Town
e-mail:
S Afr J Diabetes Vasc Dis
2013;
10
: 28–31
Painful diabetic peripheral neuropathy
HILTON KAPLAN
M
archal de Calvi gave the first description of neuropathic
pain in 1864. FW Pavy, a Guy’s Hospital physician and a
pupil of Claude Bernard, the father of modern physiology,
described in 1885 the symptoms of diabetic polyneuropathy as ‘…
of darting or lightening pains… Or there may be great pain… I have
noticed that these pains may be worse at night’ and some patients
‘could not feel properly in their legs’ and that ‘these features may
be accompanied by loss of the patellar reflexes.’
As insightful as this definition was, it did not entirely describe
neuropathic pain in the full spectrum of presentation, and the
definition of neuropathic pain presented researchers and clinicians
with difficulties.
1
However, the development and validation of
clinical tools in the form of questionnaires has been of immense
help in defining the condition and may be used in research as well
as in the clinical setting. These tools are simple and easy to use.
1
The Assessment Committee of the Neuropathic Pain Special
Interest Group NeuPSIG defined neuropathic pain (2011) as ‘pain
arising as a direct consequence of a lesion or disease affecting the
somatosensory system’. The International Association for the Study
of Pain (IASP) definition is ‘pain initiated or caused by a primary
lesion or dysfunction of the nervous system’.
The NeuPSIG definition is probably more accurate as it
distinguishes neuropathic pain from pain caused by neuroplastic
changes in the central nervous system (CNS) in response to strong
nociceptive stimulation. The term ‘somatosensory’ is used rather
than ‘nervous system’ to differentiate neuropathic pain from pain
caused by lesions in other parts of the CNS.
Peripheral neuropathy and neuropathic pain are frequent
complications of type 1 and 2 diabetes and have a similar frequency:
approximately 54–59% in type 1 and 37–45% in type 2 diabetes.
There is variability in the reported prevalence of neuropathy, ranging
from 5–80%. This probably reflects differences in population groups
studied or the diagnostic criteria used to diagnose neuropathy.
Neuropathy is usually a late finding in type 1 diabetes, but is often
an early finding in type 2 diabetes.
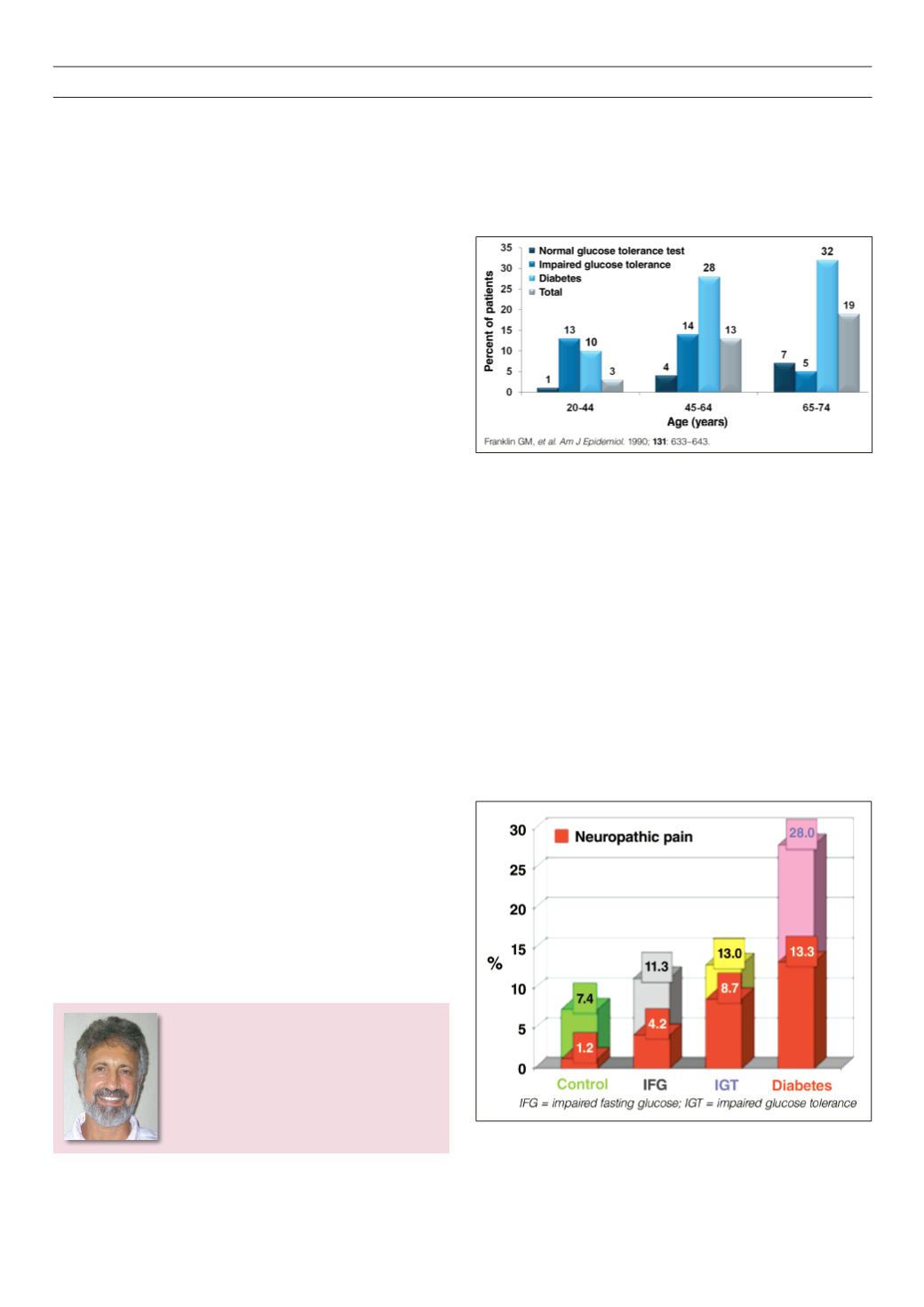
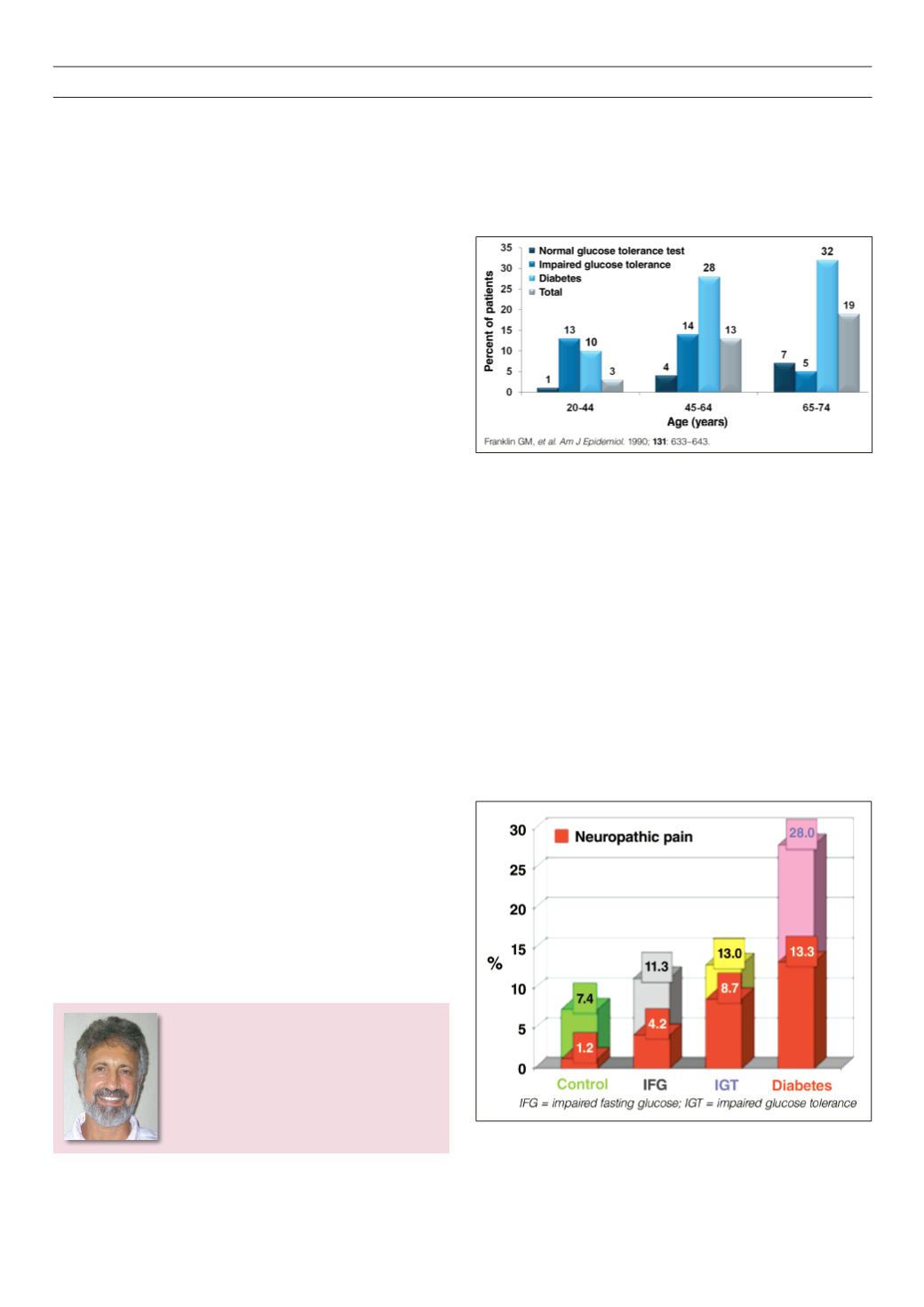
Neuropathy may also present with impaired glucose tolerance
(IGT) (Figs 1, 2). There is an increased risk with longer duration of
diabetes (Fig. 3) and also with poor glucose control.
The pathophysiological mechanisms underlying PNPD are
complex and beyond the scope of this article, other than a brief
outline. Hyperglycaemia activates several processes, resulting in
metabolic pathways contributing to polyneuropathy. These include
activation of protein kinase C beta, which in turn leads to altered
expression of endothelial nitric oxide synthetase and vascular growth
factor (VEGF), increased flux through the polyol pathway, oxidative
stress and damage caused by increased glycation of protein, and
increase in advanced glycation end-products (AGES).
Hyperglycaemia is highly correlated with the development and
progression of all neuropathies, including painful diabetic peripheral
neuropathy (PDPN). The DCCT (Diabetes Control and Complications
trial) showed that tight glycaemic control reduced the incidence
of neuropathy by 60%.
2
However, even in patients with excellent
long-term control, the lifetime incidence of PDPN remains 20%.
Strict glycaemic control is still the single most important prevention
measure for neuropathy.
The most common type of neuropathy involves the feet or hands,
in a glove or stocking pattern. The feet are much more commonly
affected than the hands. Sensory symptoms predominate, but
motor and autonomic dysfunctions often co-exist.
In the Rochester diabetes study,
3
a cross-sectional survey and
longitudinal follow up of diabetic neuropathy, 60.4% of patients
Figure 1.
Prevalence of DPN by age and glucose tolerance status.
Figure 2.
Prevalence of polyneuropathy and neuropathic pain. MONICA/KORA
Augsburg surveys S2S3.