VOLUME 10 NUMBER 1 • MARCH 2013
25
SA JOURNAL OF DIABETES & VASCULAR DISEASE
REVIEW
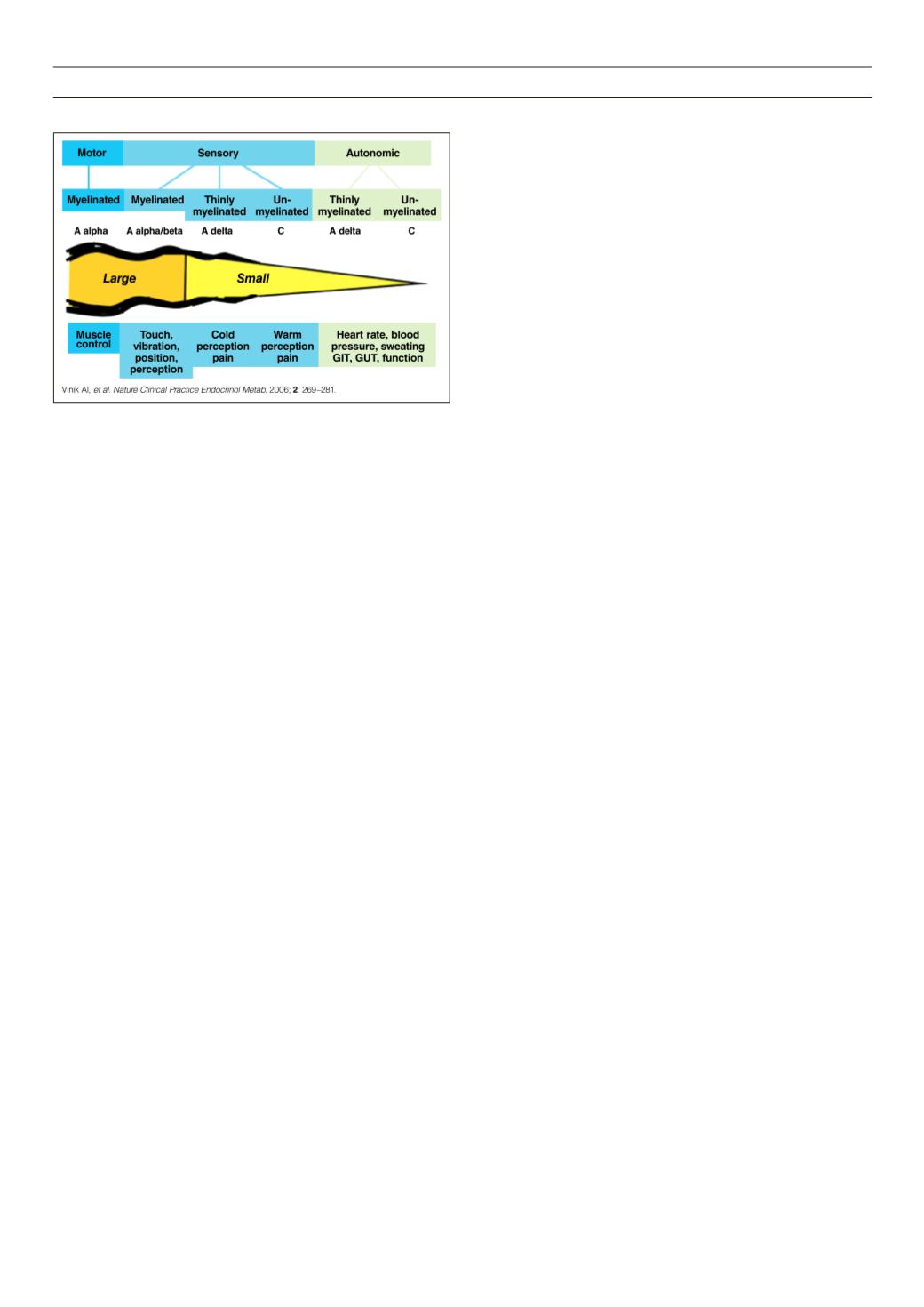
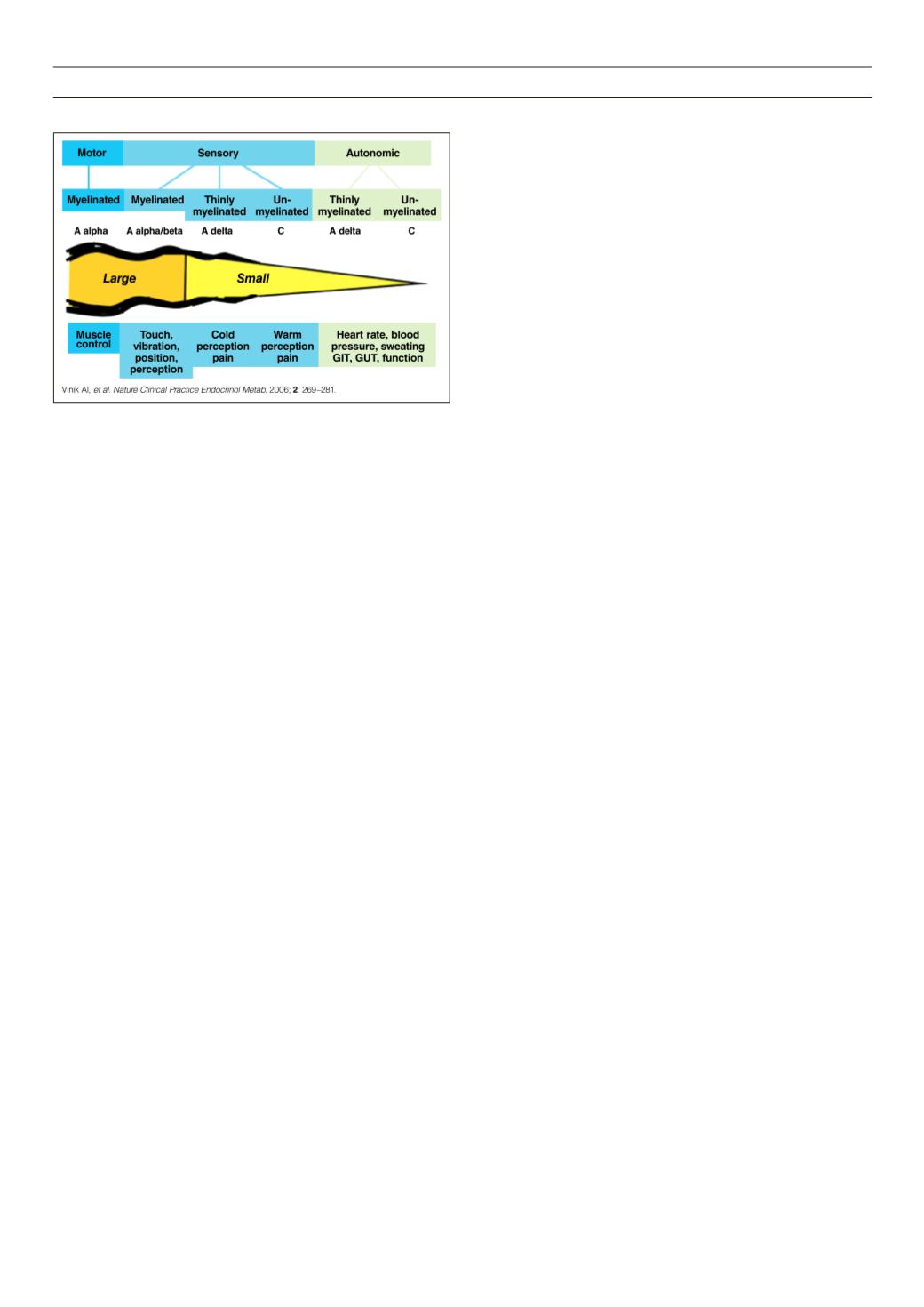
area of the nerve bundle with the small, thin myelinated and large
myelinated fibres on the periphery of the nerve bundle. Peripheral
nerve fibres conducting impuses from the periphery conduct via
large A
δ
myelinated fibres travelling at 30–70 m/s and sub-serving
touch, pressure and vibration. These fibres are considered to be
nociceptors, but due to anatomical or neurochemical changes,
these fibres may elicit pain signals.
Small myelinated A
δ
fibres travelling at a speed of 5–30 m/s
sub-serve pain in the form of pinprick and cold threshold. Small
unmyelinated C fibres conduct slowly and can respond to heat,
mechanical or chemical stimuli. Because they conduct so slowly,
standard electrophysiological neuronal testing does not reveal
damage to those A
δ
and C fibres.
Depending on the neuron type, each group of neurons responds
with slow, intermediate or rapid velocity to different stimuli and pain
thresholds. Electrical signals (action potentials) are transmitted to
the dorsal horn of the spinal cord, and then relayed via two primary
ascending pathways, the spinothalamic and spinoparabrachial
tracts, to the thalamus. The spinothalamic pathway projects into
the thalamus and somatosensory cortex. The spinoparabrachial
tract connects to the ventral medial nucleus of the hippocampus
and the central nucleus of the amygdala.
Following peripheral nerve injury, there are changes in the CNS
that contribute to the manifestation of neuropathic pain. These
changes have both a qualitative and quantitative impact on how
and where the pain is perceived. It is likely that aberrant afferent
activity is necessary for the initiation and maintenance of all aspects
of neuropathic pain associated with injury to the peripheral nervous
system.
Neuronal inflammation causes an increase in neurochemicals in
adjacent tissue. Undamaged axons distal to the site of injury are
broken down and reabsorbed by immune cells via a process termed
Wallerian degeneration. Nerve growth factor is released near the
undamaged nerve fibres and this may cause a release of tumour
necrosis factor-
α
and expression of sodium channels, transient
receptor potential vanilloid and adrenoceptors. Peripheral nerve
lesions or axonal damage can trigger an increased sodium channel
activity on C fibres.
Signal transduction is complex and involves different receptor
potential ionic channel families, e.g. the transient receptor potential
(TRP) family of ion channels, which provide the molecular basis
for thermoregulation and mechanotransduction; members of the
epithelial Na channel (ENaC) superfamily; members of the two-pore
potassium channel family; a low-voltage-gated Ca channel; and
ionotropic purinergic receptors.
The electrical stimulus then travels along the peripheral nerve to
the spinal cord. After the stimulus for pain has been transducted,
the electrical signal is conducted to the spinal cord and transmitted
to central nerves in the spinal dorsal horn. Here, signals can be
modulated (amplified or inhibited).
The signal is then conducted further until it reaches the brain,
where different brain regions process the signal (known as the pain
matrix). Only when the brain has processed the signals received
from the periphery does pain perception occur. The influence of
emotional and cognitive input and feedback from different brain
areas makes pain not only a perception but also an experience.
The dorsal horn acts as a first interface before pain signals are
conducted to the brain. Transmission of signals from the peripheral
afferent neurons to the brain is modulated by neuronal, glial and
endocrine factors.
The inhibitory mechanisms in pain processing are referred to
as the ‘gate control theory’. There is modulation of nociceptive
information by inhibitory structures, including inhibitory inter-
neurons, and descending structures from the brain at the level of
the dorsal horn. Motivational affective and cognitive factors also
influence pain modulation before pain is finally perceived and
experienced.
Many different neurotransmitters and neuromodulators are
involved in this gating process, including glutamate and substance
P, which have a facilitatory effect on signal transmission. Glutamate
is the most common facilitating agent. Substance P is released with
high-frequency input for further amplification.
Glycine,
γ
-aminobutyric acid, endocannabinoids, endorphins,
monoamines and neurosteroids exert (mainly) an inhibitory effect
on pain transmission. As well as modulation by factors in the dorsal
horn, descending inhibitory (and also facilitatory) pathways also
play a part in nociceptive signal transmission. ‘Gating’ today is used
as a term for all the processes involved in dorsal horn processing.
Within the brain there are specialised areaswhere pain is processed,
modified and finally experienced. This complex neurophysiological
process is beyond the scope of this article, but the main areas
involved in this process are the thalamus, amygdala, hippocampus,
prefrontal cortex, inferior cortex and anterior cingulate cortex. The
thalamus is the main relay station for pain input before relaying this
information on to the cortical and subcortical areas. The other areas
are involved in complex processing of information between different
parts of the brain, in memory of emotional reactions to pain, in
processing affective aspects of sensory stimulation, in placing the
painful experience into an emotionally relevant context, and in the
affective and motor responses to pain.
While affective components of pain are thought to be mainly
mediated by the medial thalamus, anterior cingulate cortex and
anterior insula, sensory aspects are attributed to the lateral thalamus,
primary and secondary somatosensory cortex, and posterior insula.
Genetics, gender and individual differences influence whether or
not a brain region is involved in pain processing.
The brain regions involved in processing pain depend on the
type of pain experienced (extreme temperature, electrical shock,
visceral). Distraction, anticipation, expectation and emotional
states also affect pain processing. The attention and perception
of pain occur in adjacent but separate sectors of the anterior
cingulate cortex.
Figure 4.
A simplified view of the PNS.