RESEARCH ARTICLE
SA JOURNAL OF DIABETES & VASCULAR DISEASE
58
VOLUME 13 NUMBER 2 • DECEMBER 2016
Results
Tables 1 and 2 show clinical and biological characteristics of
patients according to renal function. Mean age and duration of
diabetes were 58 ± 8 and 11 ± 8 years, respectively for the whole
group. BMI, waist circumference, SBP and DBP, and plasma glucose
levels averaged 26 ± 5 kg/m
2
, 95 ± 12 cm, 148 ± 26 mmHg, 84
± 13 mmHg, and 8.10 ± 3.31 mmol/l, respectively. Diabetes was
frequently associated with other CV risk factors, among which
hypertension (80%) was the commonest. Clustering of risk factors
into the metabolic syndrome was observed in 58% of patients.
Besides antidiabetic therapy, 97% of patients were receiving
BP-lowering drugs. CKD was observed in 32 patients (53%), 20 of
whom (62%) had a CrCl rate of 30 ml/min per 1.73 m
2
or higher.
Compared to those with normal renal function, the duration of
diabetes was longer (13 ± 8 vs 8 ± 6 years;
p
≤ 0.001), the proportion
of patients on current antihypertensive drugs greater (42 vs 25%;
p
< 0.05) and the level of uric acid higher (450 ± 166 vs 306 ± 107
μmol/l;
p
≤ 0.001) in CKD patients. The two subgroups were similar
for the other variables.
Table 3 summarises echocardiographic measurements by renal
function status and Table 4 by the severity of renal dysfunction.
Patients with CKD had increased LVIDD (47.00 ± 6.00 vs 43.00 ±
7.00 mm;
p
≤ 0.001), LVMI (47.00 ± 19 vs 36.00 ± 15.00 mm;
p
≤ 0.05) and higher proportions of LVH (37 vs 14%;
p
≤ 0.05);
they also showed higher proportions of concentric (22 vs 11%;
p ≤ 0.05) and eccentric (15 vs 3%;
p
≤ 0.05) LVH. Compared
to patients with moderate CKD, those with severe CKD had
increased interventricular septum thickness, diastolic (IVSD) (12.30
± 3.08 vs 9.45 ± 1.94 mm;
p
≤ 0.001), RWT (0.52 ± 0.17 vs 0.40
± 0.07 mm;
p
≤ 0.01) and higher proportions of LVH (50 vs 30%;
p
≤ 0.05). Concentric remodelling (25 vs 15%; p ≤ 0.05) and
concentric hypertrophy (42 vs 10%;
p
≤ 0.05) were the geometric
patterns most frequently encountered in patients with severe
CKD. Between groups, systolic function indices did not differ.
In multivariable adjusted analysis, the probability of LVH
among CKD patients was increased by hyperuricaemia (aOR 9.10;
95% CI: 2.40–33.74) for the presence versus the absence of
hyperuricaemia.
Discussion
The key finding of the study was that the elevated prevalence of
chronic kidney disease in our diabetic patients was associated with
abnormal cardiac structure. The alteration in renal function was
moderate in the majority of cases. Left ventricular mass index, the
frequency of left ventricular hypertrophy and uric acid levels were
higher in CKD patients in whom multivariable adjusted analysis
indicated uric acid as the only predictor of LVH.
The elevated prevalence of moderate to severe CKD has been
reported in 15 to 23% of diabetic patients in whom it predicts
the occurrence of CVD.
18,19
The mechanisms by which chronic
hyperglycaemia may induce cardiovascular and renal dysfunction
include enhanced polyol pathway flux, altered redox state,
increased formation of diacylglycerol (DAG) and subsequent
activation of protein kinase C (PKC) isoforms, and accelerated non-
enzymatic formation of advanced glycation end products (AGEs).
20
The DAG–PKC pathway affects cardiovascular and renal structure
and function in many ways, e.g. the regulation of endothelial
permeability, vascular tone, cell growth, angiogenesis, and
cytokine and leucocyte activation.
20
Moreover, insulin resistance/
hyperinsulinaemia-induced activation of the sympathetic nervous
and renin–angiotensin–aldosterone systems could contribute to
cardiovascular and renal damage through oxidative stress and
inflammation.
21-23
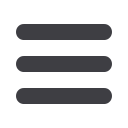
Table 3.
M-mode echocardiographic data in the whole group and
diabetics with and without CKD.
Normal renal
Whole group function
CKD
Characteristic
(
n
= 60)
(
n
= 28)
(
n
= 32)
LV dimension
LVIDD (mm)
44.83 ± 6.62
43.00 ± 7.00
47.0 ±
6.00***
LVIDS (mm)
29.67 ± 8.43
28.04 ± 7.7
2 31.09 ±
8.98
IVSD (mm)
10.42 ± 2.60
10.30 ± 2.41
11.00 ± 3.48
PWTD (mm)
9.98 ± 2.26
10.00 ± 2.00
10.00 ± 2.30
RWT
0.46 ± 0.13
0.47 ± 0.12
0.45 ± 0.13
LVMI (g/m
2
.
7
)
41.83 ± 17.72
36.00 ± 15.00
47.00 ±
19.00*
EF (%)
68.25 ± 19.06
69.24 ± 17.02
67.39 ± 20.91
FS (%)
0.34 ± 0.13
0.34 ± 0.13
0.34 ± 0.14
LV geometry
Normal (%)
43
43
44
Concentric remodelling (%) 30
43
19*
Concentric hypertrophy (%) 17
11
22*
Eccentric hypertrophy (%) 10
3
15*
Data are expressed as mean ± SD or relative frequency in per cent.
CKD, chronic kidney disease; LVIDD, left ventricular internal diameter,
diastolic; LVIDS, left ventricular internal diameter, systolic; IVSD,
interventricular
septum, diastolic; PWTD, posterior wall thickness, diastolic; RWT,
relative wall thickness; LVMI, left ventricular mass index; EF, ejection fraction;
FS, fraction shortening.
*
p
≤ 0.05; **
p
≤ 0.01; ***
p
≤ 0.001 in comparison with normal renal
function.
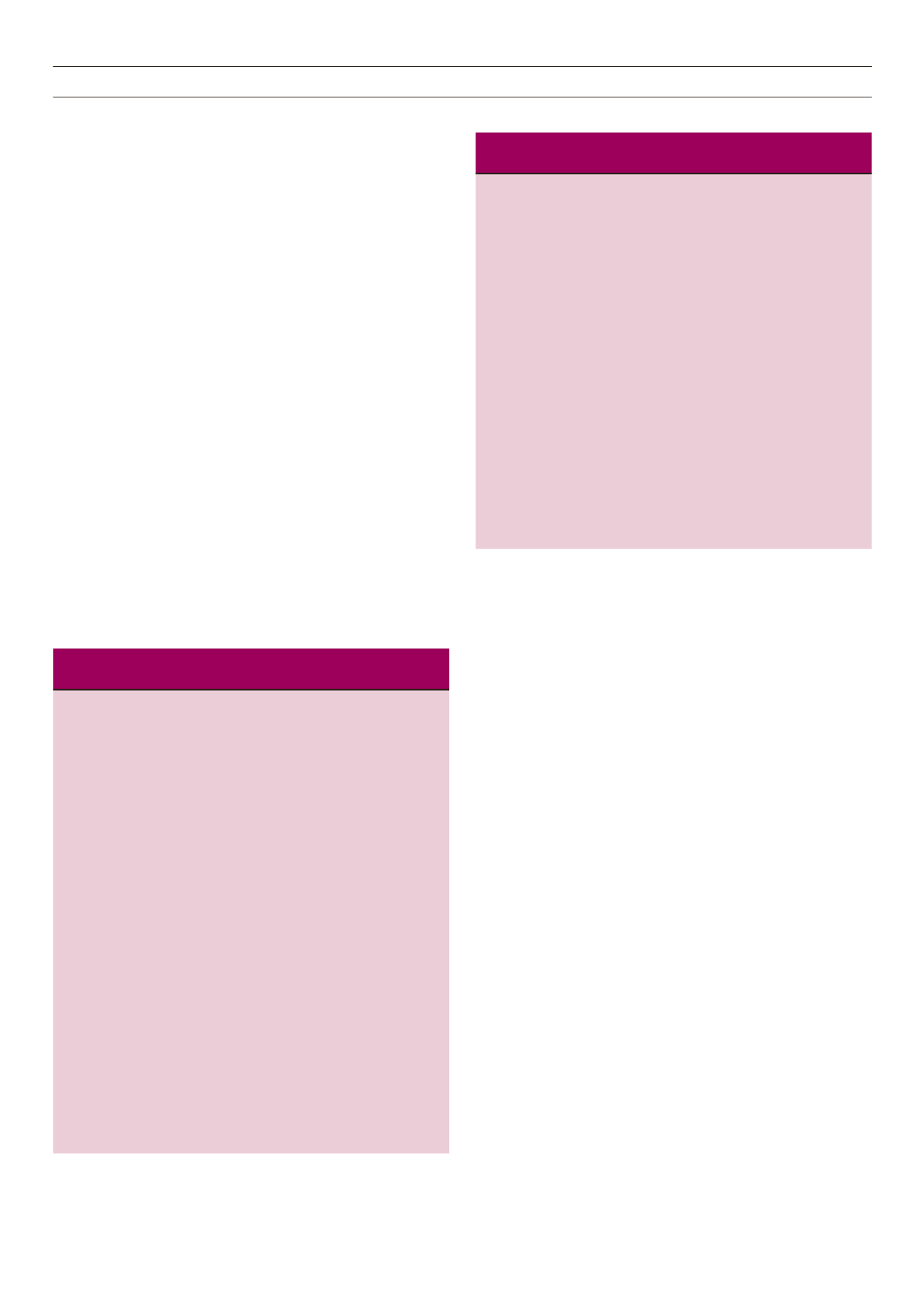
Table 4.
Severity of renal dysfunction and M-mode echocardiographic
data among diabetics with CKD.
CrCl
CrCl
30–60 ml/min < 30–60 ml/min
(
n
= 20)
(
n
= 20)
LV dimension
LVIDD (mm)
46.75 ± 5.72
46.75 ± 6.79
LVIDS (mm)
30.50 ± 9.76
32.08 ± 7.80
IVSD (mm)
9.45 ± 1.94
12.30 ± 3.08*
PWTD (mm)
9.52 ± 1.77
11.61 ± 2.78**
RWT
0.40 ± 0.07
0.52 ± 0.17**
LVMI (g/m
2
.
7
)
43.52 ± 15.74
52.41 ± 22.40
FS (%)
0.35 ± 0.15
0.32 ± 0.11
LV geometry
Normal, %
55
25*
Concentric remodelling (%)
15
25*
Concentric hypertrophy (%)
10
42*
Eccentric hypertrophy (%)
20
8*
Data are expressed as mean ± SD or relative frequency in per cent.
CKD, chronic kidney disease; CrCl, creatinine clearance; LVIDD, left
ventricular internal diameter, diastolic; LVIDS, left ventricular internal
diameter, systolic; IVSD, interventricular septum, diastolic; PWTD,
posterior wall thickness, diastolic; RWT, relative wall thickness; LVMI,
left ventricular mass index; EF, ejection fraction; FS, fraction shortening.
*
p
≤ 0.05; **
p
≤ 0.01; ***
p
≤ 0.001 in comparison with moderate CKD.



















